16 Dec Gene Additive Therapy Prevents Pain Crisis Episodes in Sickle Cell Patients
MedicalResearch.com Interview with:

Dr. Mapara
Markus Y Mapara, MD
Professor of Medicine
Director of the Blood and Marrow Transplantation
Columbia University Medical Center
MedicalResearch.com: What is the background for this study? What are the main findings?
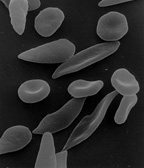
Response: Sickle cell disease is caused by a point mutation in the beta-globin gene of hemoglobin resulting in the production of abnormal hemoglobin which leads to formation of sickle-shaped RBC under conditions of low oxygen. Sickle cell disease affects about 100,000 patients in the US which are predominantly African American. The only curative approach is to perform an allogeneic bone marrow transplant which is however fraught with significant treatment-related risks if a matched sibling donor is not available.
The current study describes the successful application of a novel gene therapy to treat patients with sickle cell disease. The strategy is based on a gene-addition approach to introduce the genetic information for a Hemoglobin F-like molecule termed HgAT87Q into hematopoietic stem cells. The expression of this novel hemoglobin prevents polymerization of HgbS and has now been demonstrated to prevent the occurrence of vaso-occlusive pain crises in sickle cell disease patients.
MedicalResearch.com: How much does the therapy cost?
Response: At this point this is still investigational and there is therefore no price.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: The next big step is to achieve engraftment of genetically engineered stem cells without the need for the patient to undergo conditioning treatment in the form of high dose chemotherapy which is quite toxic. New approaches for non-myeloablative conditioning using antibody-mediated conditioning are currently under investigation in early trials and may further help to make this treatment safe and available to more patients.
Citation:
Biologic and Clinical Efficacy of LentiGlobin for Sickle Cell Disease Gene Therapy
DOI: 10.1056/NEJMoa2117175
MedicalResearch.com is not a forum for the exchange of personal medical information, advice or the promotion of self-destructive behavior (e.g., eating disorders, suicide). While you may freely discuss your troubles, you should not look to the Website for information or advice on such topics. Instead, we recommend that you talk in person with a trusted medical professional.
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on December 16, 2021 by Marie Benz MD FAAD
