11 Apr Prenatal Exposure to SSRIs May Be Linked to Changes in Infant Brain Development
MedicalResearch.com Interview with:
Jiook Cha, PhD
Assistant Professor
Division of Child and Adolescent Psychiatry
Columbia University Medical Center
New York, NY 10032
MedicalResearch.com: What did we already know about the connection between maternal SSRI use during pregnancy and infant brain development, and how do the current study findings add to our understanding? What’s new/surprising here and why does it matter for mothers and babies?
Response: Prior studies have shown mixed results in terms of the associations between maternal SRI use during pregnancy and offspring’s brain and cognitive development. Neurobiological studies with animal models suggest that SSRI use perturbs serotonin signaling and that this has important effects on cognitive development (a study conducted an author of this paper, Jay Gingrich, MD, PhD: Ansorge et al., 2004, Science). The human literature has been more mixed in terms of the associations of prenatal exposure to SSRI with brain and cognitive development.
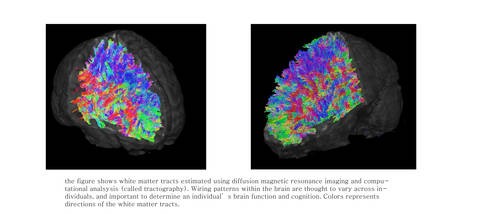
In our study, we used neonatal brain imaging because this is a direct, non-invasive method to test associations between SSRI use and brain development at an early developmental stage, limiting the effects of the post-natal environment. In our study, we had two different control groups, that is, a non-depressed SSRI-free group (healthy controls), and depressed but SSRI-free (SSRI controls) group. Also, in our study we used rigorous imaging analytics that significantly improve the quantitative nature of MR-derived signals from the brain structure using two of the nation’s fastest supercomputers (Argonne National Laboratory and Texas Advanced Computing Center) and allows robust reconstruction of brain’s grey and white matter structure in the infants’ brains.
We report a significant association of prenatal exposure to SSRI with a volume increases within many brain areas, including the amygdala and insula cortex, and an increase in white matter connection strength between the amygdala and insular cortex. We were surprised by the magnitude of the effects (or the statistical effect size), compared with other brain imaging studies in psychiatry with children or adults’ brains. Importantly, it should be noted that our estimates of brain structure are still experimental and for research-purpose only. This means that our data need to be replicated and rigorously tested against confounders in order to make a firm conclusion. While our study suggests a “potential” association between prenatal exposure to SSRI and a change in fetal or infant brain development, we still need more research.
MedicalResearch.com: Can you please explain in very simple terms what happens in the body and brain when pregnant women use SSRIs that might alter brain development in babies, and to what extent we know if the infant brain development is being impacted by the drugs versus by the severity of their mothers’ depression?
Response: Serotonin is an important neurotransmitter in general, but its effects are more broad-spread in the fetal brain relative to the adult brain. Animal studies indicate that during the fetal period, serotonin acts as an essential neurotrophic factor – that is, it plays an important role in initial brain development. Though we do not fully know, we do know that this critical development is strictly governed by the precise molecular and cellular mechanisms. When pregnant women use SSRIs in their brains serotonin levels increase. What is unknown is whether, and to what extents serotonin levels within the fetal brains change in response to prenatal exposure to SSRI. If there is no change, it is possible that prenatal exposure to SSRI has no effects on fetal development. If there is a change, it is possible that prenatal exposure to SSRI has an effect on fetal development. Our study supports the latter case; on the other hand, some prior studies support the former.
It becomes much more complicated if considering the impact of mothers’ depression. It is very difficult to imagine that a single study can demonstrate the complex impact of prenatal exposure to SSRI, maternal depression, and an interaction between the two on fetal development, as well as long-term brain and cognitive development. The current science does not sufficiently explain this. We need more research.
We address the issue of disentangling the effects of maternal depression from that of prenatal SSRI exposure in our response to question 3.
MedicalResearch.com: Based on the findings of this study and other research to date on SSRIs during pregnancy, what do you see as the benefits and harms of maternal SSRI use during pregnancy for both mothers and for babies?
Response: Based on our study and those of other researchers, we can say with some confidence that SSRI medications have an influence of fetal brain development. Exactly what that influence means over the longer term with regard to the infant’s cognitive and emotional development remains unclear and requires subsequent research to really understand.
Prior research on SSRI medications and fetal brain development was limited in its ability to disentangle the effects of maternal depression from that of prenatal SSRI exposure. We designed this study to (statistically) control for the effects of maternal depression, providing a clearer picture of the effects of SSRI exposure.
Whereas potential SSRI effects on fetal brain development are concerning, maternal depression is also an important factor that influences the fetus and the mother. Maternal depression increases the risk for negative pregnancy outcomes such as low birth weight and prematurity. It can also lead to post-partum depression with effects on mother-infant bonding.
An important take home message from our study is that there are still a lot of unanswered questions about the effects on maternal SSRI use during pregnancy and additional research is sorely needed.
MedicalResearch.com: Do you think women should use SSRIs during pregnancy, and if so, which women should take these drugs while pregnant and what alternative options might some women have to manage depression without taking SSRIs?
Response: If a pregnant woman becomes depressed, getting treatment is very important. Several options are available including medications and psychotherapies. Deciding which treatment option is the best for any individual patient is a decision between that patient and her doctor. The pros and cons of the treatment options need to be considered in the context of the individual patient. More rigorous scientific research is required to aid such decisions.
Citations:
[wysija_form id=”3″]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on April 11, 2018 by Marie Benz MD FAAD