MedicalResearch.com Interview with:
Catherine M. Stein, PhD
MedicalResearch.com Interview with:
Catherine M. Stein, PhD
Associate professor of epidemiology and biostatistics
Case Western Reserve
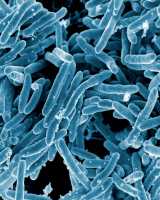
Dr. Stein is a leader of international research on resistance to
Mycobacterium tuberculosis (
MTB) infection
MedicalResearch: What is the background for this study? What do you hope to learn?
Dr. Stein: In a 2002 study, we began to clinically characterize people who lived in households where there were infectious tuberculosis cases. We followed them for a two-year period and noticed that approximately 9 percent of household members were resistant to
Mycobacterium tuberculosis (
MTB) infection, even though they were highly exposed to the organism. This finding surprised us because the prevailing notion had been that everyone living in TB-endemic settings or living with someone who has TB would become infected eventually. After several years of study, we found a substantial number of these people who do not have any evidence for
MTB infection, so we wanted to do studies to learn if we could figure out why.
MedicalResearch: Is MTB resistance a new phenomenon? Do MTB resisters react to a tuberculin purified protein derivative (PPD) or a gold immunoassay but don’t develop clinical disease?
Dr. Stein: We don’t have any reason to believe that
MTB-infection resistance is a new phenomenon. It’s just that no one has thought to look for it before. In terms of the PPD or gold immunoassays,
MTB-resisters produce a negative response to both tests. The way gold immunoassays are done, three tubes are collected. One is a control. Another is a test for reacting to
MTB. Still another is a positive control to make sure immune cells are alive. The
MTB-resisters show a response to that positive control but not to
MTB. It’s not that these patients don’t have an immune response. It’s just that they have no response to
MTB, which means they have no previous exposure to cause their T-cells to make that response.
MedicalResearch: Are MTB-resisters immune to the newer multi-drug resistant strains of TB?
Dr. Stein: Resistance to MTB infection is independent of the drug resistance pattern of the bacteria. Thus we would expect them to resist multidrug resistant (MDR)-TB as well. There is no strong evidence that MDR-TB is more aggressive or virulent.
(more…)