23 Mar Cognitive Outcomes of Prenatal Exposure to Opioid Use Disorder Medications
MedicalResearch.com Interview with:
Leah Nelson, MD MS
Addiction Medicine Fellow
University of New Mexico
MedicalResearch.com: What is the background for this study?
Response: With the progression of the opioid epidemic over the past decade, more women of reproductive age are seeking treatment for addiction. Many more pregnant women are prescribed methadone and buprenorphine, two opioid medications that prevent relapse and overdose. Maternal use of mediations for opioid use disorder is recommended because it lowers the risk to the fetus from uncontrolled drug use and also allows the mother to engage with prenatal care and social work. Subsequently, the number of infants born after prenatal exposure to opioids is increasing.
Several previous studies have shown measurable differences in the cognitive scores of children after prenatal opioid exposure. However, much of the previous work was done on convenience samples (easy to recruit rather than rigorously matched for comparability) and the demographic characteristics of both mothers and children in the exposed and unexposed groups varied widely on important factors such as maternal education, socioeconomics, employment, tobacco use, and infant gender. Each of these factors has been demonstrated to impact early childhood development in the absence of opioid exposure.
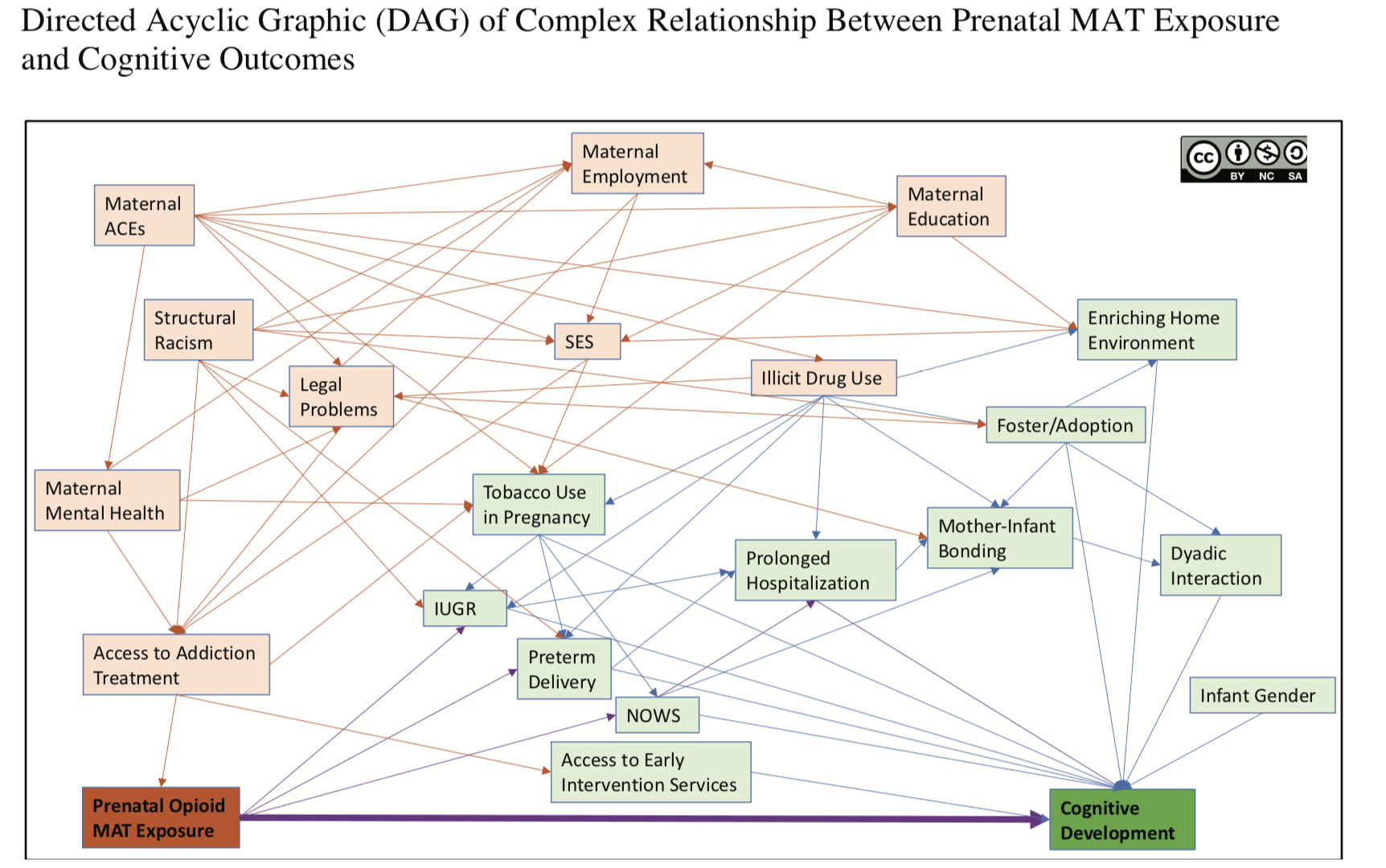
ACEs = adverse childhood experiences, IUGR= intrauterine growth restriction, MAT= medication assisted therapy, SES = socioeconomic status
The above graphic attempts to illustrate a proposed relationship between prenatal opioid exposure and impacts on cognitive development. The exposure is “Prenatal Opioid MAT exposure” in the dark orange box. The outcome of interest is “Cognitive Development” in the dark green box. The question is whether the exposure causes the outcome (bold purple line directly connecting these two boxes). As shown, there are many upstream factors (orange boxes) that influence the likelihood of fetal exposure to opioid MAT. These maternal factors are connected via biasing pathways (orange lines) to factors known to influence on cognitive development (green boxes). Not all possible relationships are shown. Relatively few causal pathways (purple lines) are present in the diagram to connect the exposure and outcome.
This work is licensed by Leah Nelson, MD under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/ or send a letter to Creative Commons, PO Box 1866, Mountain View, CA 94042, USA
MedicalResearch.com: What are the main findings?
Response: Our study was interested in the cognitive outcomes (learning, memory, verbal skills, etc) of young children born after medication for opioid use disorder exposure controlled for comparability. We therefore conducted a meta-analysis of about 50 years of research. We pooled the data to look for effects with a larger sample and made an effort to compare studies with better matching of exposed and unexposed groups. As with previous reports, we found a small but statistically significant trend toward lower cognitive scores for children with prenatal methadone and buprenorphine exposure in the overall analysis, but the finding was highly heterogenous. High heterogeneity indicates the studies did not have similar findings, and thus the results of the meta-analysis must be interpreted with caution. Most of the sub-analyses on maternal demographics also had high heterogeneity. However, one sub-analysis of four studies found that when maternal tobacco use during pregnancy was similar between opioid-exposed and unexposed children, the cognitive effect approached zero, became non-significant, and was homogenous, indicating a high reliability of the result.
MedicalResearch.com: What should readers take away from your report?
There are two main take-home messages for this study:
- Opioid use during pregnancy may or may not have direct cognitive impacts for the developing child. The poor recruitment of comparable groups by previous studies prevents us from being able to draw conclusions about the cognitive impacts even with meta-analysis.
- Smoking cessation should be a priority during prenatal care for women with opioid use disorder because of the well-established risks of smoking while pregnant.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: Future addiction research needs to prioritize high quality design and strict recruitment standards to avoid biased conclusions. Given the known effects of prenatal and early childhood environment on development, researchers cannot ignore recruitment variables such as maternal education, mental health, experiences of trauma, racism, socioeconomics, employment, hospital length of stay, mother-child bonding, dyadic relationship, foster care and adoption, concurrent exposures to other medication, drugs, or tobacco, among a myriad of other life experiences that impact both the mother and child. Funding agencies should ensure that study design is rigorous with respect to recruitment variables during the grant review and approval process.
MedicalResearch.com: Is there anything else you would like to add?
Response: Efforts to alleviate inequity, prevent addiction, and improve access to evidence-based addiction treatment should take priority for all women, particularly those from racially and ethnically underserved populations who bear a disproportionate burden of the risk factors for addiction.
Early intervention services should be offered to all families with opioid exposed infants in order to promote healthy growth and development.
No disclosures.
Citation:
[subscribe]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on March 23, 2020 by Marie Benz MD FAAD