01 Nov Lung Cancer: Stanford Risk-Based Model Reduces Screening Disparities
MedicalResearch.com Interview with:

Dr. Han
Summer S Han, PhD
Associate Professor
Quantitative Sciences Unit
Stanford Center for Biomedical Informatics Research (BMIR)
Department of Neurosurgery and Department of Medicine
Department of Epidemiology & Population Health (by Courtesy)
Stanford University School of Medicine

Dr. Choi
Dr. Eunji Choi PhD
Instructor, Neurosurgery
Department: Adult Neurosurgery
Stanford University School of Medicine
MedicalResearch.com: What is the background for this study?
- Lung cancer is the leading cause of cancer death in the United States, killing about 127,000 people annually, but it can be treatable if detected early.
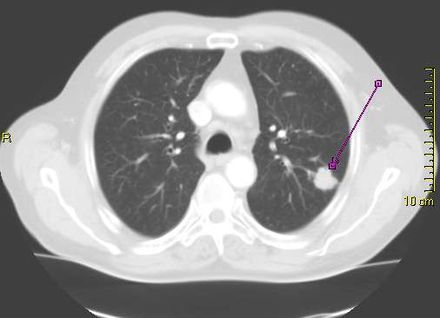
- Low-dose computed tomography, or CT scan, has been shown to significantly reduce the number of lung cancer deaths. But because the radiation delivered by the scans can be harmful (they use on average about 10 times the radiation of standard X-rays), only those people at relatively high risk for lung cancer should be screened. The two biggest risk factors for lung cancer are exposure to tobacco smoke and age. Current national guidelines that rely on age and smoking exposure to recommend people for lung cancer screening are disproportionally failing minority populations including African Americans, according to a new study led by researchers at Stanford Medicine.
- In 2021, the national guidelines by the U.S. Preventive Services Task Force (USPSTF) issued revised recommendation guidelines on lung cancer screening, lowering the start age from 55-year to 50-year and the smoking pack-year criterion from 30 to 20, compared to the 2013 USPSTF criteria. In comparison to the 2013 criteria, the new modifications have been shown to lessen racial disparities in screening eligibility between African Americans and Whites. However, potential disparities across other major racial groups in the U.S., such as Latinos, remains poorly examined.
- Meanwhile, risk prediction model assesses a person’s risk score of developing an illness, such as lung cancer.
MedicalResearch.com: What are the main findings?
Response: The study found that an alternative risk-based method that incorporates additional information including family history and other health problems such as previous cancer diagnoses does a better job of eliminating disparities among races.
MedicalResearch.com: What should readers take away from your report?
- In this study, researchers from Stanford University used an ideal metric to evaluate racial disparities in lung cancer screening in five major racial and ethnic groups in the U.S.
- To better capture racial disparity, the screening eligibility to incidence ratio (E-I ratio) was estimated in each racial group based on a large prospective cohort from the Multiethnic Cohort Study (MEC).
- The E-I ratio: the number of people in a group eligible for screening compared with the number of lung cancer cases found in that group over a certain time.
- Higher E-I ratios imply adequate screening (i.e., screening adequately covers the lung cancer population).
- Lower E-I ratios reflect underserved screening, implying that some lung cancer cases occur in people who were not deemed eligible for screening.
- The metric indicates significantly underserved screening (eligibility) despite the high lung cancer risk (incidence) among African American adults versus White adults (E-I ratio: 9.5 vs 20.3, respectively) under the USPSTF criteria.
- The disparity between African American and White adults was substantially reduced (E-I ratio: 15.9 vs. 18.4, respectively), with minimal disparities observed in other races, including Latino, Asian, and Native Hawaiian adults, said lead author Summer Han, Ph.D., associate professor in Department of Neurosurgery at Stanford School of Medicine.
- Further analysis showed that selecting people to screen based on the risk-based analysis was more likely than the task force guidelines to accurately identify people with lung cancer — a measure known as sensitivity — and fewer screens were needed to detect one case of lung cancer (26 versus 30).
MedicalResearch.com: What recommendations do you have for future research as a results of this study?
- Disparities evident in the U.S. Preventive Services Task Force’s lung cancer screening guidelines may have a significant impact on lung cancer mortality in the United States. We clearly show that a method that incorporates additional information in screening assessments is better at identifying true cases of lung cancer. It also reduces the number of false positives.
- Thus, the findings suggest that incorporating risk model-based lung cancer screening strategies should be considered for future recommendations to eliminate racial disparities in lung cancer early detection via screening programs.
- The researchers hope that their findings will spur a national dialogue about race-based disparities in lung cancer screening recommendations and how to devise more equitable and effective guidelines.
Disclosures: The study was funded by the National Institutes of Health (grants 4R37CA226081 and 1R01CA282793) and the Stanford Cancer Institute.
Citation:
Choi E, Ding VY, Luo SJ, et al. Risk Model–Based Lung Cancer Screening and Racial and Ethnic Disparities in the US. JAMA Oncol. Published online October 26, 2023. doi:10.1001/jamaoncol.2023.4447
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition.
Some links may be sponsored. Products are not endorsed.
Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on November 1, 2023 by Marie Benz
