10 Apr Collagen Biomarker Associated With Atrial Fibrillation and Heart Failure Risk
MedicalResearch.com Interview with:
Susana Ravassa PhD
Program of Cardiovascular Diseases, CIMA
University of Navarra, and IdiSNA
Navarra Institute for Health Research
Pamplona, Spain
MedicalResearch.com: What is the background for this study?
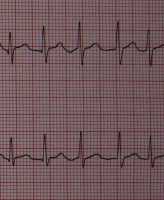
Response: Atrial fibrillation (AF) is an evolving epidemic responsible for substantial morbidity, mortality and health-care expenditure. In particular, when AF and heart failure (HF) occur in combination, clinical evolution is particularly poor. Left atrial (LA) myocardial interstitial fibrosis (MIF) is the main structural lesion in AF and considered as the main factor responsible for the perpetuation of this pathology. In addition, it is known that MIF is associated with a lower effectiveness of the treatment of AF by pulmonary vein isolation with catheter ablation. Therefore, the identification of biomarkers related to MIF, as an affordable and minimally invasive approach, is of great interest to detect patients at risk of AF, as well as to monitor their response to the LA ablation therapy.
We had previously demonstrated that the deleterious impact of MIF in the heart is due to alterations in both the quality (i.e., extent of cross-linking among collagen fibrils and type of collagen fibers that determine their rigidity and resistance to degradation [collagen cross-linking or CCL]) and the quantity (i.e., extent of collagen fibers that occupy the myocardial tissue [collagen deposition or CD]) of fibrotic tissue. We have shown that certain circulating biomarkers related to collagen type I metabolism are associated with CCL and CD. On the one hand, the serum carboxy-terminal propeptide of procollagen type I (PICP), released during the conversion of procollagen type I into fibril-forming mature collagen type I, is directly correlated with myocardial CD.
On the other hand, the ratio of serum carboxy-terminal telopeptide of collagen type I to serum matrix metalloproteinase-1 (serum CITP:MMP-1 ratio) is inversely correlated with myocardial CCL, as the higher is the cross-linking among collagen type I fibrils the lower will be the cleavage of CITP by MMP-1 during the process of degradation of the fiber. Interestingly, we have previously reported that the combination of these biomarkers identifies patients with heart failure presenting with a complex pattern of MIF characterized by both increased CCL and CD (CCL+CD+) showing a higher risk of adverse clinical evolution as compared with heart failure patients without this combination of biomarkers. As both increased CCL and CD have been found in the left atrial myocardium in patients with AF, we designed this investigation to explore whether the CCL+CD+ combination of biomarkers is associated with AF.
MedicalResearch.com: What are the main findings?
Response: The most important findings of this study are the following: the CCL+CD+ combination of biomarkers is associated with the prevalence of AF and with a higher risk of developing new-onset AF in patients with heart failure. In addition, the CCL+CD+ combination is associated with larger left atrium low-voltage areas and with a lower effectiveness of the catheter ablation therapeutic approach in patients with heart failure. These results indicate that a complex type of MIF characterized by both increased collagen type I cross-linking and increased collagen type I deposition determines the risk of atrial fibrillation in HF patients, and identifies those patients at high risk of atrial fibrillation recurrence after ablation, suggesting that this complex pattern of MIF is responsible for maintaining an arrhythmogenic substrate refractory to the catheter ablation procedure in atrial fibrillation patients.
MedicalResearch.com: What should readers take away from your report?
Response: This investigation supports an important notion: the assessment of a combination of circulating biomarkers of increased myocardial collagen type I cross-linking and deposition (i.e. CCL+CD+) may identify patients carrying a pattern of complex MIF that are at high risk of developing AF, as well as at high risk of AF recurrence after ablation. Therefore, the CCL+CD+ bioprofile identified in this study sheds light on the pathophysiology of the association of MIF with AF as it reinforces the notion that the complexity of MIF resulting from alterations in both the properties and the amount of the deposited collagen fibers seem to be relevant for this association. In addition, the fact that AF recurrence is particularly high in AF patients with the CCL+CD+ bioprofile suggests that the efficacy of the AF ablation procedure is not optimal in patients with a high myocardial deposition of highly cross-linked collagen type-I fibers, opening up the possibility of utilizing this combination of biomarkers to consider the convenience of catheter ablation in these patients and the utilization of additional therapies.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: We need to move forward with further studies to determine ease of testing and generalizability of the relation found between the CCL+CD+ bioprofile and the presence and future development of AF to larger cohorts/populations. In addition, further investigation is required to establish whether patients carrying the CCL+CD+ combination of biomarkers may benefit from specific therapeutic strategies aimed to correct these alterations of collagen metabolism at the myocardial level and, in turn, to reduce the risk of development of atrial fibrillation or the risk of post-ablation AF recurrence. In this regard, we are currently working on the design of a multicenter randomized study to analyze these aspects.
MedicalResearch.com: Is there anything else you would like to add?
Response: This work includes a substudy to evaluate the association of the CCL+CD+ bioprofile with the eletroanatomical properties of the left atria evaluated by high resolution electroanatomic maps. This precise technique reveals that CCL+CD+ patients exhibit larger low voltage areas in the left atria as compared with the remaining AF patients, which is universally considered as a sign of fibrosis or scar. Therefore, we have demonstrated a direct link between the CCL+CD+ bioprofile with the electrical damage responsible for the AF occurrence and maintenance. In this regard, Dr Ignacio García-Bolao has received consultant, proctoring and speaker’s fees from Boston Scientific Corporation, owner of the high density mapping system used to evaluate the electrical properties of the left atria in these patients.
Citation:
Journal of the American College of Cardiology
Volume 73, Issue 12, April 2019 DOI: 10.1016/j.jacc.2018.12.074
Combination of Circulating Type I Collagen-Related Biomarkers Is Associated With Atrial Fibrillation
Susana Ravassa, Gabriel Ballesteros, Begoña López, Pablo Ramos, Jean Bragard, Arantxa González, María U. Moreno, Ramón Querejeta, Enrique Vives, Ignacio García-Bolao and Javier Díez
[wysija_form id=”3″]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on April 10, 2019 by Marie Benz MD FAAD
