Author Interviews, Heart Disease, JACC / 05.02.2021
Identifying Cardiac Strain Early May Minimize Heart Failure in Chemotherapy Patients
MedicalResearch.com Interview with:
Paaladinesh Thavendiranathan MD, SM
Ted Rogers Centre for Heart Research and the Division of Cardiology
Peter Munk Cardiac Center, University Health Network,
Joint Department of Medical Imaging, , University Health Networ
Toronto, Ontario, Canada
MedicalResearch.com: What is the background for this study?
Response: Anthracyclines are a common class of chemotherapy drugs used to treat patients with blood, breast, and many other cancers. Patients receiving anthracycline based cancer therapy who are deemed to be high cardiovascular risk either based on their age or presence of cardiovascular risk factors are at risk of developing heart failure. In high risk patients this risk of heart failure could be between 5-10% over a 5 year period depending on the treatment regimens used. Therefore it is possible that the cancer patient of today can become a heart failure patient of tomorrow. These cancer treatments are however very effective against the cancer. So it is important to find strategies to prevent the development of heart failure. Usually oncologists and cardiologists work together to monitor patients during and after cancer therapy using surveillance strategies.
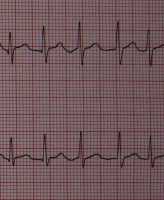
One such strategy is to repeat heart ultrasounds to identify heart dysfunction early followed by initiation of cardioprotective therapy. Traditional approaches measure left ventricular ejection (LVEF) as a metric of heart function. However, we have learned that with this approach it may be too late when a change in LVEF is identified. Global longitudinal strain (GLS) is a newer echocardiography method that appears to identify heart dysfunction earlier before a major change in LVEF occurs. However, whether initiation of cardioprotective therapy when a change in GLS is identified can prevent a reduction in heart function and development of cardiotoxicity (significant change to heart function) is unknown.
The SUCCOUR trial is an international, multicenter randomized controlled trial that compared using an LVEF based approach to surveillance (arm 1) versus the addition of GLS based surveillance (arm 2) in high risk patients receiving anthracycline based therapy. The study enrolled 153 patients in the LVEF arm and 154 patients in the GLS arm. Majority of the patients (~90%) had breast cancer. (more…)






 Deborah M Eaton
Doctorate Student / Research Assistant
Temple University
MedicalResearch.com: What is the background for this study?
Response: Heart failure (HF) with preserved ejection fraction (HFpEF) accounts for approximately 50% of cases of HF and to date clinical trials with HFpEF patients have failed to produce positive outcomes. Part of this is likely due to the lack of HFpEF animal models for preclinical testing. Our lab addressed this gap in knowledge by developing an animal model that mimics critical features of the human HFpEF phenotype. We performed an in-depth cardiopulmonary characterization highlighting that the model has characteristics of human disease. We then tested the effects of a pan-HDAC inhibitor, vorinostat/SAHA, in collaboration with Dr. Timothy McKinsey, who is an expert in HDAC inhibitors and recently published work1 that laid the foundation for this study.
Deborah M Eaton
Doctorate Student / Research Assistant
Temple University
MedicalResearch.com: What is the background for this study?
Response: Heart failure (HF) with preserved ejection fraction (HFpEF) accounts for approximately 50% of cases of HF and to date clinical trials with HFpEF patients have failed to produce positive outcomes. Part of this is likely due to the lack of HFpEF animal models for preclinical testing. Our lab addressed this gap in knowledge by developing an animal model that mimics critical features of the human HFpEF phenotype. We performed an in-depth cardiopulmonary characterization highlighting that the model has characteristics of human disease. We then tested the effects of a pan-HDAC inhibitor, vorinostat/SAHA, in collaboration with Dr. Timothy McKinsey, who is an expert in HDAC inhibitors and recently published work1 that laid the foundation for this study.