15 Apr Is Immediate Cardioversion Necessary in New Onset Atrial Fibrillation?
MedicalResearch.com Interview with:
Harry J.G.M Crijns, MD, PhD
University Hospital Maastricht
Maastricht, The Netherlands
MedicalResearch.com: What is the background for this study? What are the main findings?
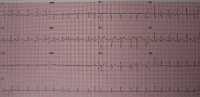
Response: An episode of the heart rhythm disorder ‘atrial fibrillation’ is a frequent reason for a visit to the Emergency Department. Patients commonly undergo a cardioversion to restore sinus rhythm – either electrical or pharmacological. However, it is known that episodes of atrial fibrillation frequently terminate spontaneously. Therefore, we conducted a multicenter randomized clinical trial in the Netherlands, researching whether a wait-and-see approach – consisting of heart rate slowing drugs and cardioversion only if the heart rhythm does not resolve spontaneously – was non-inferior to the current standard of care of immediate cardioversion.
The primary end point was the presence of sinus rhythm on the ECG at the 4 weeks visit, which was present in 91% in the wait-and-see approach and 94% in the standard of care, which was within the non-inferiority margin.
In the wait-and-see approach, 69% of patients returned to sinus rhythm spontaneously, i.e. without cardioversion. Complications were rare and comparable in both treatment arms, and the percentage of patients experiencing a recurrence of atrial fibrillation during the first 4 weeks after the index visit was comparable (30% vs 29% respectively). We concluded that in patients presenting to the emergency department with recent-onset, symptomatic atrial fibrillation, a wait-and-see approach was non-inferior to early cardioversion in achieving a return to sinus rhythm at 4 weeks.
MedicalResearch.com: What should readers take away from your report?
Response: Recent-onset symptomatic atrial fibrillation usually terminates spontaneously and therefore an acute cardioversion is not always necessary, as a wait-and-see approach is equally effective and safe. Quality of life is the same in both treatment options. Physicians should discuss with their patients which one of the two approaches – wait-and-see or immediate cardioversion – would be more suitable in their situation.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: Now that we have shown that early, i.e. immediate cardioversion may not be necessary, we are planning future studies on how to implement a delayed cardioversion into daily practice.
MedicalResearch.com: Is there anything else you would like to add?
Response: Funding for this trial was provided by the Netherlands Organization for Health Research and Development, and Boehringer Ingelheim.
Citation:
Early or Delayed Cardioversion in Recent-Onset Atrial Fibrillation
Nikki A.H.A. Pluymaekers, M.D., Elton A.M.P. Dudink, M.D., Ph.D., Justin G.L.M. Luermans, M.D., Ph.D., Joan G. Meeder, M.D., Ph.D., Timo Lenderink, M.D., Ph.D.,
Jos Widdershoven, M.D., Ph.D., Jeroen J.J. Bucx, M.D., Ph.D.,
Michiel Rienstra, M.D., Ph.D., Otto Kamp, M.D., Ph.D.,
Jurren M. Van Opstal, M.D., Ph.D., Marco Alings, M.D., Ph.D.,
Anton Oomen, M.D., and Harry J.G.M. Crijns, M.D., Ph.D
et al., for the RACE 7 ACWAS Investigators*
March 18, 2019
DOI: 10.1056/NEJMoa1900353
[wysija_form id=”3″]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on April 15, 2019 by Marie Benz MD FAAD
