Author Interviews, Breast Cancer, Cancer Research, JAMA, Race/Ethnic Diversity / 09.03.2023
Triple-Negative Breast Cancer: Racial and Ethnic Disparities Vary Between US States
MedicalResearch.com Interview with:
 Hyuna Sung, PHD
Senior Principal Scientist, Cancer Surveillance Research
American Cancer Society
Kennesaw, GA 30144
MedicalResearch.com: What is the background for this study?
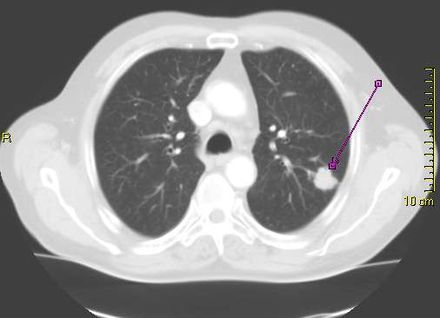
Response: Triple-negative breast cancer (TNBC) accounts for 10% to 20% of all breast cancer diagnoses in the US.
This subtype of breast cancer tends to spread faster and has fewer treatment options. In the US, Black women are about two-fold more likely than White women to develop TNBC.
(more…)
Hyuna Sung, PHD
Senior Principal Scientist, Cancer Surveillance Research
American Cancer Society
Kennesaw, GA 30144
MedicalResearch.com: What is the background for this study?
Response: Triple-negative breast cancer (TNBC) accounts for 10% to 20% of all breast cancer diagnoses in the US.
This subtype of breast cancer tends to spread faster and has fewer treatment options. In the US, Black women are about two-fold more likely than White women to develop TNBC.
(more…)
 Hyuna Sung, PHD
Senior Principal Scientist, Cancer Surveillance Research
American Cancer Society
Kennesaw, GA 30144
Hyuna Sung, PHD
Senior Principal Scientist, Cancer Surveillance Research
American Cancer Society
Kennesaw, GA 30144