MedicalResearch.com Interview with:
Christine Greene, Ph.D. and Chuanwu Xi, Ph.D.
School of Public Health, Department of Environmental Health Sciences
University of Michigan
Medical Research: What is the background for this study?
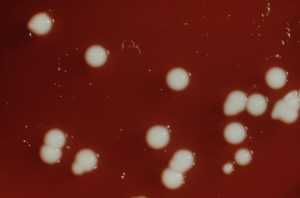
Response: Healthcare-associated infections (HAIs) are a serious problem globally. A
cinetobacter baumannii, a gram-negative opportunistic pathogen, was mostly unheard of 10-15 years ago, but is now a clinically significant pathogen in hospitals.
A. baumannii causes a variety of infections ranging from urinary tract infections to bacteremia and patients who are at high risk of
A. baumannii infection are those who are critically ill, who have indwelling catheters or patients with long hospital says. Once infected, the risk of mortality is high – up to 26% for in-hospital patients and as much as 43% for those in the ICU. The mortality rate is high largely due to the rapid ability for this pathogen to develop antibiotic resistance. Despite patient isolation, we still see hospital outbreaks because
A. baumannii survives very well in the environment and it is resistant to most biocides, detergents, dehydration, and UV radiation.
A. baumannii is also a known biofilm former. Biofilms serve to protect the microorganism. In the open environment, biofilms protect from desiccation and other harsh environmental insults such as biocides, thereby promoting persistence in the open environment. In the human body, biofilms protect against the immune system, provide an additional layer of protection from antibiotics and contribute to reoccurring infections in the patient.
This research characterizes the fitness (desiccation tolerance) trade-offs imposed on
A. baumannii isolated from clinical and environmental settings. This investigation compares isolates of
A. baumannii from both environments on the basis of multidrug resistance, biofilms and desiccation tolerance. We looked to see if either MDR or biofilm formation increased fitness (ability to tolerate desiccation) or impose a fitness cost depending on environmental conditions.
Medical Research: What are the main findings?
Response: We provide evidence of variation in desiccation tolerance between clinical and environmental isolates of similar phenotypes and show a trend of increased desiccation tolerance for high biofilm forming
clinical isolates with additional tolerance when the ability to form biofilms is coupled with the multidrug resistance. By contrast, biofilm formation had a significant impact on desiccation tolerance for
environmental isolates.
(more…)










![MedicalResearch.com Interview with: Gili Regev-Yochay, MD, Lead author Director of the Infection Prevention & Control Unit Sheba Medical Center Tel HaShomer, Israel. MedicalResearch.com: What is the background for this study? Response: CPE (Carbapenemase producing Enterobacteriaceae) is endemic in Israel. In our ICU we had a prolonged CPE outbreak with one particular bacteria, which is not that common (OXA-48 producing-Serratia marcescens). Enhancing our regular control measures (hand hygiene, increased cleaning etc..) did not contain the outbreak. MedicalResearch.com: What are the main findings? Response: The outbreak source were the sink-traps in nearly all the patient rooms, which were contaminated with this same bacteria. Once we understood that this was the source we took two measures: 1) Sink decontamination efforts, including intensive chlorine washes of the drainage and water system, replacement of all sink-traps, acetic acid treatment and more, all these efforts were only partially and only temporarily successful. So that even today, after a year of such efforts and a period in which we didn't have any patients with this infection, the drainage system is still contaminated with these bugs and they grow in the sink-traps and can be found in the sink outlets. 2) The second measure we took was an educational intervention, where we engaged the ICU team through workshops to the issue of the contaminated sinks and together enforced strict "sink-use guidelines" (sinks are to be used ONLY for hand washing, prohibiting placement of any materials near the sinks, etc.). Using these two measure the outbreak was fully contained. To date, nearly 1.5 years since the last outbreak case, we did not have any further infections in our ICU patients with this bug. MedicalResearch.com: What should readers take away from your report? Response: Sink-traps and drainage systems can be a major source of CPE transmission. While traditionally CPE outbreaks were attributed to patient-to patient transmission, the environment and particularly water and drainage system appears to play a major role. MedicalResearch.com: What recommendations do you have for future research as a result of this work? Response: There is urgent need to find a technological solution for drainage system contaminations. While some have suggested to get rid of sinks in ICU this is probably not realistic in the era of emerging Clostridium infections (where washing hands, and not only alcohol rubs are needed). Citation: Gili Regev-Yochay, Gill Smollan, Ilana Tal, Nani Pinas Zade, Yael Haviv, Valery Nudelman, Ohad Gal-Mor, Hanaa Jaber, Eyal Zimlichman, Nati Keller, Galia Rahav. Sink traps as the source of transmission of OXA-48–producing Serratia marcescens in an intensive care unit. Infection Control & Hospital Epidemiology, 2018; 1 DOI: 1017/ice.2018.235 [wysija_form id="3"] [last-modified] The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.](https://medicalresearch.com/wp-content/uploads/sink.jpg)
![MedicalResearch.com Interview with: Gili Regev-Yochay, MD, Lead author Director of the Infection Prevention & Control Unit Sheba Medical Center Tel HaShomer, Israel. MedicalResearch.com: What is the background for this study? Response: CPE (Carbapenemase producing Enterobacteriaceae) is endemic in Israel. In our ICU we had a prolonged CPE outbreak with one particular bacteria, which is not that common (OXA-48 producing-Serratia marcescens). Enhancing our regular control measures (hand hygiene, increased cleaning etc..) did not contain the outbreak. MedicalResearch.com: What are the main findings? Response: The outbreak source were the sink-traps in nearly all the patient rooms, which were contaminated with this same bacteria. Once we understood that this was the source we took two measures: 1) Sink decontamination efforts, including intensive chlorine washes of the drainage and water system, replacement of all sink-traps, acetic acid treatment and more, all these efforts were only partially and only temporarily successful. So that even today, after a year of such efforts and a period in which we didn't have any patients with this infection, the drainage system is still contaminated with these bugs and they grow in the sink-traps and can be found in the sink outlets. 2) The second measure we took was an educational intervention, where we engaged the ICU team through workshops to the issue of the contaminated sinks and together enforced strict "sink-use guidelines" (sinks are to be used ONLY for hand washing, prohibiting placement of any materials near the sinks, etc.). Using these two measure the outbreak was fully contained. To date, nearly 1.5 years since the last outbreak case, we did not have any further infections in our ICU patients with this bug. MedicalResearch.com: What should readers take away from your report? Response: Sink-traps and drainage systems can be a major source of CPE transmission. While traditionally CPE outbreaks were attributed to patient-to patient transmission, the environment and particularly water and drainage system appears to play a major role. MedicalResearch.com: What recommendations do you have for future research as a result of this work? Response: There is urgent need to find a technological solution for drainage system contaminations. While some have suggested to get rid of sinks in ICU this is probably not realistic in the era of emerging Clostridium infections (where washing hands, and not only alcohol rubs are needed). Citation: Gili Regev-Yochay, Gill Smollan, Ilana Tal, Nani Pinas Zade, Yael Haviv, Valery Nudelman, Ohad Gal-Mor, Hanaa Jaber, Eyal Zimlichman, Nati Keller, Galia Rahav. Sink traps as the source of transmission of OXA-48–producing Serratia marcescens in an intensive care unit. Infection Control & Hospital Epidemiology, 2018; 1 DOI: 1017/ice.2018.235 [wysija_form id="3"] [last-modified] The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.](https://medicalresearch.com/wp-content/uploads/sink-200x150.jpg)