Author Interviews, Heart Disease, JAMA, NYU, USPSTF / 02.02.2022
USPSTF: Screening for Atrial Fibrillation in Adults over 50
MedicalResearch.com Interview with:
Gbenga Ogedegbe, MD, MPH
Dr. Adolph & Margaret Berger Professor of Population Health
Director, Division of Health & Behavior
Director Center for Healthful Behavior Change
Department of Population Health
NYU Langone Health
NYU School of Medicine
Member of the U.S. Preventive Services Task Force
MedicalResearch.com: What is the background for this study? What are the main findings?
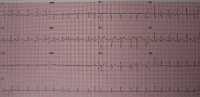
Response: Atrial Fibrillation (AFib) is the most common type of irregular heartbeat and a major risk factor for stroke, and it often goes undetected. For this recommendation, the Task Force evaluated whether screening adults over the age of 50 who do not have any signs or symptoms of AFib can help prevent strokes.
In its evidence review, Task Force expanded its scope to include a search for studies on portable and wearable devices such as smartphones and fitness trackers in addition to electrocardiography (ECG). Despite this consideration, the Task Force found insufficient evidence to recommend for or against screening for AFib. This is consistent with the Task Force’s 2018 recommendation.
(more…)