Author Interviews, Critical Care - Intensive Care - ICUs, Genetic Research, Pediatrics / 10.03.2025
Optimized Care Improves Survival of Infants with Severe Genetic Bone Disorder, Osteogenesis imperfecta
MedicalResearch.com Interview with:
Ricki S. Carroll, MD
Complex Care and Palliative Care Physician, Skeletal Dysplasia and Palliative Care Teams
Nemours Children’s Hospital
Wilmington, Delaware
MedicalResearch.com: What is the background for this study?
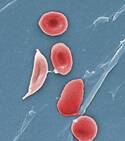
Response: Individuals with Osteogenesis imperfecta (OI) are often classified into one of four subtypes: type I (mild/nondeforming), type II (perinatal lethal), type III (severe/progressively deforming) and type IV (moderately deforming); however, this classification system continues to evolve with increasing knowledge (Sillence, 1979; Van Dyke & Sillence, 2014). Those with a mild phenotype are often diagnosed postnatally or in the pediatric setting after experiencing multiple unexplained fractures. Concerns for moderate to severely presenting OI are often noted in utero when fractures, shortening, and/or bowing of the long bones are found on prenatal ultrasound (Marini et al, 2017).
When Osteogenesis imperfecta is suspected and/or molecularly confirmed in the prenatal period, families may be counseled that the diagnosis is lethal or severely life-limiting based on prenatal ultrasound observations and previously reported genotype-phenotype correlations (Yoshimura et al., 1996; Krakow et al., 2009). Ultrasound parameters for predicting lethality in skeletal dysplasias have been studied and include the chest-to-abdominal circumference ratio of <0.6 and femur length-to-abdominal circumference ratio of <0.16 (Yoshimura et al., 1996; Rahemtullah et al., 1997; Ramus et al., 1998). However, there are nuances to this strategy, for instance in cases where bowing deformities and fractures limit the accuracy of true femur length measurements (Milks et al., 2017). While genotype-phenotype correlations are also considered when predicting lethality, there can be a range of clinical variability even among those with the same genotype (Rauch et al., 2004, Marini et al, 2017). Some specialized delivery centers have reported on the accuracy of these methods in predicting lethality, yet many of the pregnancies evaluated are ultimately terminated, further limiting the ability to draw conclusions (Yeh et al., 2011). These limitations pose a challenge for perinatal providers counseling families on the diagnosis and attempting to prognosticate postnatal survival probability. Consequently, this information can cloud conversations surrounding delivery planning and influence access to potential life-saving therapies including invasive mechanical ventilation and feeding support.
Advancements in medical technology and the option for life-sustaining interventions have significantly altered the prognoses for severely affected infants. In this manuscript, we describe perinatal outcomes of infants referred to a single specialized center after receiving a prior diagnosis of possibly lethal, lethal or type II OI where parents sought medical intervention after birth. We also outline advances in respiratory and feeding support needs, as well as length-of-stay for these neonates. The success of this multidisciplinary approach to neonatal OI care both challenges previously defined expectations for this patient population and offers a chance at survival.
(more…)