Author Interviews, JAMA, Mental Health Research, Pediatrics, Social Issues / 13.04.2022
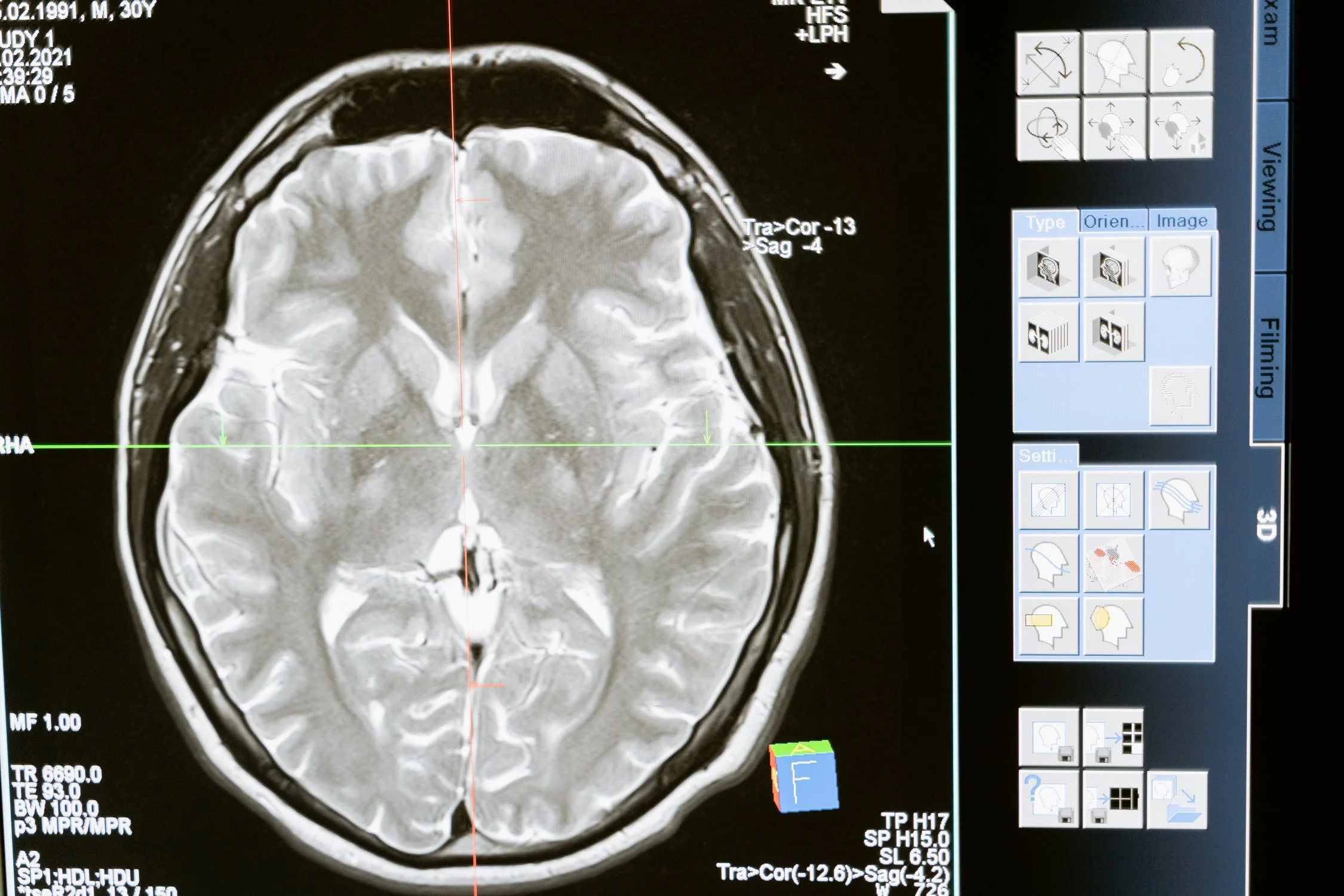
Poverty During Pregnancy Associated with Reduced Infant Brain Size
MedicalResearch.com Interview with:
Regina Triplett, M.D., M.S.
Developmental Neuroscience Post-Doctoral Research Scholar
Department of Neurology
Washington University in St. Louis, MO
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: This is an ongoing, longitudinal, prospective study of 399 pairs of mothers studied throughout pregnancy and their infants, designed to investigate exposure to early life adversity (prenatal poverty and stress) on infant brain development and behavior in early childhood. We examined measures of maternal socioeconomic status including neighborhood factors and stress/mental health during pregnancy in relation to data from infant brain MRI scans conducted in the first weeks after birth.
We found that poverty during pregnancy is associated with reduced size and folding of infant brains. We found these associations across the whole brain and not specific to one region.
(more…)