30 Sep Risk of Stroke Acutely Elevated by Episodes of Paroxysmal Atrial Fibrillation
MedicalResearch.com Interview with:

Dr. Singer
Daniel E. Singer, MD
Professor of Medicine, Harvard Medical School
Professor in the Department of Epidemiology
Harvard T.H. Chan School of Public Health
Division of General Internal Medicine
Massachusetts General Hospital
Boston, MA, 02114
MedicalResearch.com: What is the background for this study?
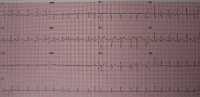
Response: Atrial fibrillation (AF) raises the risk of ischemic stroke 4-5-fold and this risk is largely reversible by oral anticoagulants (OAC). These facts are part of the core knowledge of internal medicine and the basis of multiple guidelines. They are based on studies of patients with persistent or predominantly “heavy burden” paroxysmal AF completed in the 1990s.
More recent studies using cardiac implantable devices (CIEDs: implantable defibrillators, pacemakers, etc) which have the capacity to monitor heart rhythm continuously have found that many older patients have brief, often undiagnosed, episodes of AF. Several of these studies have found that strokes occur during periods of sinus rhythm temporally distant from a preceding episode of AF. This has led to a widespread suspicion that AF is not a direct causal risk factor but a risk “marker” indicating the presence of other truly causal features like a diseased left atrium (atrial myopathy). If the risk marker hypothesis is correct, then long-term anticoagulation is needed even for brief and rare episodes of AF (assuming the patient’ s CHA2DS2-VASc score is high enough). The key problem with prior prospective studies using CIEDs was that only a small number of strokes were observed leading to inadequate statistical power.
Our study addressed this power problem by linking the very large Optum electronic health record database which could identify ischemic strokes with the Medtronic CareLink database of long-term, continuous heart rhythm records of patients with CIEDs. We ended up studying 891 individuals who had an ischemic stroke and had 120 days of continuous heart monitoring prior to the stroke.
MedicalResearch.com: What are the main findings?
- We found a tight temporal association between episodes of AF and stroke risk. The risk of stroke is acutely elevated by episodes of paroxysmal AF (PAF) and decreases rapidly (by 30 days to be conservative) after the end of the episode.
- Multihour episodes of AF on a given day are needed to raise stroke risk. We tested 5.5 hours on a given day but the strongest association we found was for >23 hours on a given day in a 30-day period. Our findings are not precise but they strongly suggest that short episodes of AF don’t raise stroke risk significantly.
MedicalResearch.com: What should readers take away from your report?
- The traditional view that AF acutely raises the risk of stroke is supported by our findings. Our work makes it unlikely that episodes of AF raise the risk of stroke months after the episode has ended, i.e., during long periods of sinus rhythm. From a mechanistic point of view, AF appears to be a cause of stroke, not just a marker of other causes of ischemic stroke.
- It appears to take longer episodes of AF to raise stroke risk. It is unclear what the exact threshold is to raise stroke risk. ≥5.5 hours of AF on a given day clearly raised stroke risk but the strongest effect we observed was for >23 hours on a given day during a 30-day period.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: Most importantly, we need a randomized trial of time-delimited, fast onset DOAC anticoagulation for patients with infrequent episodes of AF (and a qualifying CHA2DS2-VASc score, e.g., ≥2) and continuous heart rhythm monitoring.
Disclosures: I receive research support from Bristol Myers Squibb. I have consulted for Bristol Myers Squibb and for Pfizer, the manufacturers of apixaban anticoagulant. I also consult for Fitbit.
Citation:
Singer DE, Ziegler PD, Koehler JL, Sarkar S, Passman RS. Temporal Association Between Episodes of Atrial Fibrillation and Risk of Ischemic Stroke. JAMA Cardiol. Published online September 29, 2021. doi:10.1001/jamacardio.2021.3702
[subscribe]
[last-modified]
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Last Updated on September 30, 2021 by Marie Benz MD FAAD
