Author Interviews, Clots - Coagulation, Heart Disease, Karolinski Institute, Kidney Disease / 06.10.2022
Study Finds Reduced Kidney Disease Progression with DOACs vs Vitamin K Antagonists
MedicalResearch.com Interview with:
Juan Jesus Carrero Pharm PhD
Professor of Epidemiology
Cardio-renal Department of Medical Epidemiology and Biostatistics
Karolinska Institutet, Stockholm
MedicalResearch.com: What is the background for this study? What are the main findings?
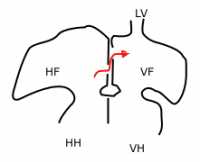
Response: Concerns on the possibility of (direct oral anticoagulants) DOAC-related nephropathy may limit its use.
In this cohort study of non-valvular AF patients from routine clinical practice, initiation of DOAC vs (vitamin K antagonists) VKA was associated with more favorable kidney outcomes, i.e., a lower risk of the composite of kidney failure and sustained 30% eGFR decline, as well as a lower risk of AKI occurrence.
In agreement with trial evidence, we also showed that DOAC vs VKA treatment was associated with a lower risk of major bleeding, but a similar risk of the composite of stroke, systemic embolism or death.
(more…)