MedicalResearch.com Editors' note: Please consult your health care provider before initiating any vitamin supplementation, including Vitamin D as potentially serious side effects are possible.
MedicalResearch.com Interview with:
Prof. Ilkka T Harvima
Department of Dermatology
University of Eastern Finland and Kuopio University Hospital
Kuopio, Finland
MedicalResearch.com: What is the background for this study?
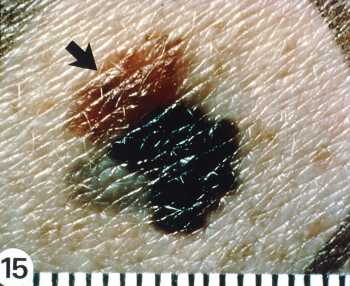
Response: The North Savo Skin Cancer Program in Eastern Finland was launched in 2017, and it aims at reducing the incidence, morbidity and mortality caused by skin cancers, such as basal cell carcinoma, squamous cell carcinoma and melanoma. A part of this program constituted a follow-up project of patients with an assessed risk of skin cancer. There are also several other parts, such as analysis of skin cancer material reposited in the Biobank of Eastern Finland (see the enclosed BMC Cancer 2021 reference), public information, education of general physicians and medical students etc.
In 2021, we published the article in BMC Cancer (enclosed), where we attempted to clarify the reasons for the relatively high melanoma mortality in relation to its incidence in this region (North Savo) of the country. By using the biobank material we also published an article in 2022 showing that melanoma and melanoma in situ associate with keratinocytic premalignant lesions and keratinocyte skin carcinomas (Suhonen V, Siiskonen H, Suni M, Rummukainen J, Mannermaa A, Harvima IT. Malignant and in situ subtypes of melanoma are associated with basal and squamous cell carcinoma and its precancerous lesions. Eur J Dermatol 2022 Apr 1;32(2):187-194. doi: 10.1684/ejd.2022.4221.).
The follow-up study of about 500 subjects is ongoing (COVID-19 caused pretty much trouble for the recruitment). This is focused on finding risk factors and biomarkers for skin cancers and carcinogenesis.
The first study on these follow-up patients was published in 2021 (Komulainen J, Siiskonen H, Harvima IT. Association of elevated serum tryptase with cutaneous photodamage and skin cancers. Int Arch Allergy Immunol 2021;182(11):1135-1142. doi: 10.1159/000517287.).
The article on vitamin D just recently published in Melanoma Research on Dec 28, 2022, is the second one.
The third work in pipeline deals with the association of atopic disorders with skin cancers, and the manuscript is under revision.
So, these provide with some background for the article in Melanoma Research. Actually, we thought that vitamin D use might associate with skin photoaging, actinic keratoses and carcinogenesis, but the only, though very important, finding was its association with melanoma. We have not focused our research just on vitamin D only, but it looks like we need to go further.
(more…)