Author Interviews, Heart Disease, JAMA, Lipids / 21.08.2020
Younger Patients with Atherosclerotic Heart Disease Less Likely To Receive Aspirin or Statins
MedicalResearch.com Interview with:
First Author
Dhruv Mahtta, DO, MBA
Cardiovascular Disease Fellow
Baylor College of Medicine
Houston, TX
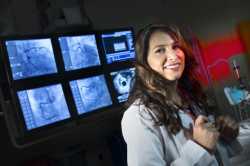
Senior & Corresponding Author
Salim S. Virani, MD, PhD, FACC, FAHA, FASPC
Professor, Section of Cardiovascular Research
Director, Cardiology Fellowship Training Program
Baylor College of Medicine
Staff Cardiologist, Michael E. DeBakey Veterans Affairs Medical Center
Co-Director, VA Advanced Fellowship in Health Services Research & Development
Michael E. DeBakey VA Medical Center, Houston, TX
MedicalResearch.com: What is the background for this study?
Response: The incidence of atherosclerotic cardiovascular disease among young patients has been on the rise. These patients with premature and extremely premature atherosclerotic cardiovascular disease experience similar rates of mortality compared to older adults. Additionally, these young patients have a greater accrued rate of life-time morbidity. Therefore, secondary prevention measures such as use of guideline concordant statin therapy and aspirin therapy are paramount in this population. (more…)