Addiction, Author Interviews, Mental Health Research / 31.03.2025
Does evergreening contribute to the prescribing pattern of citalopram and escitalopram to U.S. Medicaid and Medicare patients?
Parita K. Ray
Medical Student
Department of Medical Education
Geisinger College of Health Sciences
Scranton, PA 18509
MedicalResearch.com: What is the background for this study?
- Citalopram and escitalopram are two of the most commonly prescribed antidepressants in the U.S. and are widely used for treating major depressive disorder (MDD) and generalized anxiety disorder (GAD), along with various off-label indications. While both medications share similar mechanisms of action, escitalopram was introduced as a purified version of citalopram’s active enantiomer. Despite little evidence showing a clear superiority of escitalopram over citalopram in efficacy or tolerability, prescribing trends appear to favor escitalopram, raising concerns about "evergreening"—a practice where pharmaceutical companies promote newer formulations of existing drugs to extend market exclusivity. Prior research has shown variations in the prescription rates of psychotropic medications across states and within specific populations, particularly among Medicaid and Medicare patients. However, little is known about the long-term prescribing patterns of citalopram versus escitalopram in these populations and whether these trends reflect potential evergreening practices.







 Elena Stains
Medical Student
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA
MedicalResearch.com: What is the background for this study?
Response: Opioid use has been an increasing problem since the early 2000s in the United States (US) with a surge around 2010. Twenty-five percent of those having abused pain relievers in 2013 and 2014 got those drugs from physicians1. Physicians are particularly well-known for fueling the opioid crisis in Florida in the 2000s. Of the United States’ top 100 opioid prescribing physicians in 2010, an astounding 98 were prescribing in Florida2. Florida taking the main stage of the opioid crisis can be attributed to several factors, including ability of physicians to dispense opioids directly from their offices to patients (i.e. without pharmacists) and the presence of many infamous “pill mills” in the state3–6.
The researchers at Geisinger Commonwealth School of Medicine aimed to analyze the amount of hydrocodone (including brand names of Vicodin and Lortab) and oxycodone (OxyContin and Percocet) distributed in Florida from 2006 to 2021, paying close attention to the peak year of the opioid crisis, 2010. The team used the Washington Post and the US Drug Enforcement Administration’s Automation of Reports and Consolidated Orders System (ARCOS) databases to compile this compelling information.
Elena Stains
Medical Student
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA
MedicalResearch.com: What is the background for this study?
Response: Opioid use has been an increasing problem since the early 2000s in the United States (US) with a surge around 2010. Twenty-five percent of those having abused pain relievers in 2013 and 2014 got those drugs from physicians1. Physicians are particularly well-known for fueling the opioid crisis in Florida in the 2000s. Of the United States’ top 100 opioid prescribing physicians in 2010, an astounding 98 were prescribing in Florida2. Florida taking the main stage of the opioid crisis can be attributed to several factors, including ability of physicians to dispense opioids directly from their offices to patients (i.e. without pharmacists) and the presence of many infamous “pill mills” in the state3–6.
The researchers at Geisinger Commonwealth School of Medicine aimed to analyze the amount of hydrocodone (including brand names of Vicodin and Lortab) and oxycodone (OxyContin and Percocet) distributed in Florida from 2006 to 2021, paying close attention to the peak year of the opioid crisis, 2010. The team used the Washington Post and the US Drug Enforcement Administration’s Automation of Reports and Consolidated Orders System (ARCOS) databases to compile this compelling information.






 Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
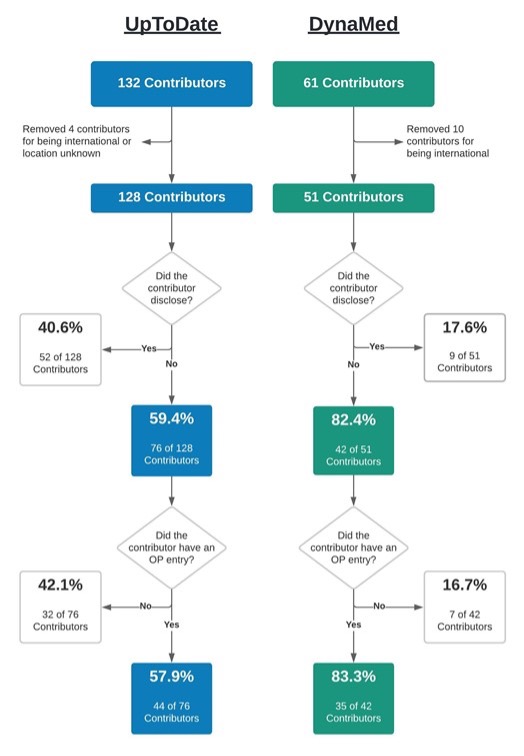
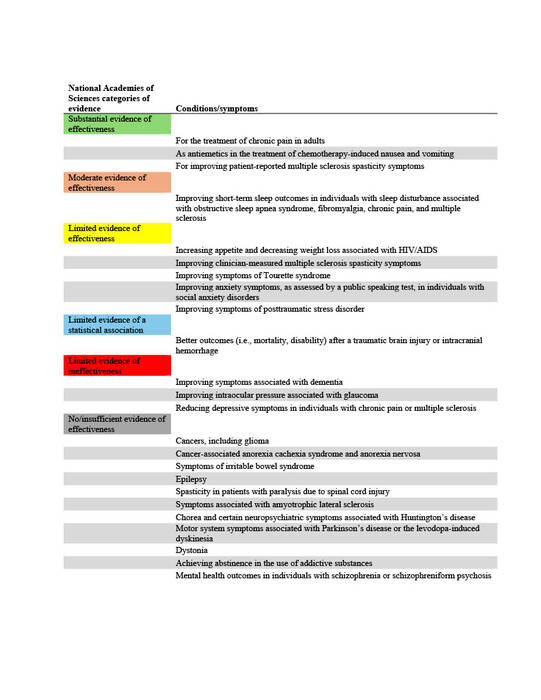
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.
Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.