MedicalResearch.com Interview with:
Daniel Maloney, Ph.D
Farrar Lab
Smurfit Institute of Genetics
Trinity College Dublin
MedicalResearch.com: What is the background for this study? Would you briefly describe the condition of Dominant optic atrophy?
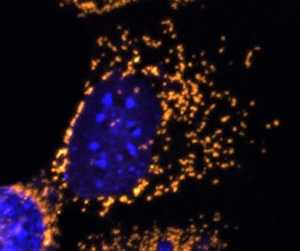
Response: Dominant Optic Atrophy (DOA) is a progressive blinding disorder that affects roughly 1:10,000 to 1:30,000 people. It is primarily caused by mutations in the OPA1 gene, which plays a pivotal role in the maintenance of the mitochondrial network. There is currently no way to prevent or cure DOA. We sought to build upon previous work to test if OPA1 could be delivered as a potential gene therapy intervention. (more…)
Author Interviews, Cannabis, Ophthalmology, Race/Ethnic Diversity, Social Issues / 09.11.2020
Ophthalmology: Identifying Racial and Socioeconomic Disparities in Eye Health
MedicalResearch.com Interview with:
Joshua Uhr MD
Ophthalmologist
Philadelphia, PA
MedicalResearch.com: What is the background for this study?
Response: Disparities in American society have been at the forefront of the public consciousness in recent months. As part of the larger discussion about inequality, disparities in health outcomes have received much attention. In light of the renewed recognition that these disparities are stark and widespread, we felt it important to evaluate disparities in our own field, ophthalmology.
Previous studies have shown disparate outcomes for individual eye conditions, such as glaucoma, cataract, and retinal detachment. Although the common and relevant endpoint of these is visual impairment, few prior studies have examined disparities in visual impairment more broadly. Our aim was to provide an updated analysis of disparity in visual impairment among adults in the United States based on race and socioeconomic status. (more…)
Author Interviews, Cognitive Issues, Mediterranean Diet, NIH / 21.04.2020
Effect of Mediterranean Diet on Cognitive Function in Patients with Age-Related Eye Disease
MedicalResearch.com Interview with:
Emily Y. Chew, M.D.
Director of the Division of Epidemiology and Clinical Applications
Deputy Clinical Director at the National Eye Institute (NEI),
National Institutes of Health
MedicalResearch.com: What is the background for this study?
Response: Dementia is a common disorder that was estimated to have a worldwide prevalence of 44 million in 2016 and is projected to hit 115 million by 2050. Many phase 3 trials of various therapies have failed and we have no treatment currently available for the prevention or reduction of the course of dementia. A slow neurocognitive decline throughout life is part of the normal process of aging. However, there is a subset of individuals who may have accelerated aging and is at high risk of development dementia. If the course of such accelerated decline could be altered in any way, it would be important to evaluate. The role of diet with biologic aging has been studied and diet has been also found to be associated with age-related conditions linked to dementia, including cardiovascular disease and diabetes.
We were interested in the cognitive function of our participants who had another neurodegenerative disease, age-related macular degeneration (AMD). We had conducted two randomized controlled clinical trials designed to evaluate the role of oral supplements for the treatment of AMD. We also studied cognitive function in both clinical trials of nearly 8,000 participants who were followed for 10 years. We also evaluated the dietary habits of the participants with food frequency questionnaires (FFQ) at baseline. Cognitive function testing was conducted in the first study, the Age-Related Eye Disease Study (AREDS) near the end of the clinical trial while the AREDS2, the second study, evaluated cognitive function testing at baseline and every 2 years until year 6. AREDS study evaluated cognitive function with in-clinic study visits while AREDS2 was conducted using telephone interviews.
Our aim was to determine whether closer adherence to the alternative Mediterranean diet (aMED) was associated with impaired cognitive function these two studies. We were interested in the particular components of the Mediterranean diet that may be important. We also evaluated the interaction of genetics with the diet. (more…)
Author Interviews, Endocrinology, Ophthalmology, Thyroid Disease / 06.04.2020
Teprotumumab-Tepezza Reduces Proptosis in Patients with Thyroid Eye Disease
MedicalResearch.com Interview with:
Dr. Raymond Douglas MD PhD
Board Certified Oculoplastic Surgeon
Beverly Hills, CA
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by proptosis? How does teprotumumab work?
Response: This study provides pooled efficacy data from the Phase 2 and 3 clinical trials of teprotumumab showing that the recently FDA-approved medicine effectively reduces proptosis, also known as eye bulging, in patients with Thyroid Eye Disease (TED) regardless of age, gender and smoking status. Proptosis is one of the most debilitating symptoms of TED, especially given the accompanying pain, vision impairment and emotional distress.
Teprotumumab is a fully human monoclonal antibody and a targeted inhibitor of the IGF-1 receptor. In patients with Thyroid Eye Disease, the IGF-1 receptor is overexpressed on orbital tissues and when activated, causes inflammation and enlargement of ocular muscles, expansion of orbital tissue and fat and forward displacement of the eye, resulting in eye bulging. The proteins in teprotumumab target and bind to the IGF-1 receptor and inhibit its function, thereby reducing inflammation, preventing tissue expansion behind the eye, and preventing muscle and fat tissue remodeling. Based on this mechanism of action, it is believed that teprotumumab addresses the underlying biology of the disease. (more…)
Author Interviews, JAMA, Ophthalmology, Rheumatology / 15.12.2019
Examination of Nailfold Capillaries Can Unmask Systemic Nature of Exfoliation Glaucoma
MedicalResearch.com Interview with:
Robert Ritch, MD, FACS, FARVO
Shelley and Steven Einhorn Distinguished Chair
Professor of Ophthalmology, Surgeon Director Emeritus
Chief, Glaucoma Services Emeritus
The New York Eye and Ear Infirmary of Mount Sinai
New York, NY 10003
Founder, Medical Director and
Chairman, Scientific Advisory Board
The Glaucoma Foundation
MedicalResearch.com: What is the background for this study?
Response: Nailfold capillaroscopy (NFC), long used in rheumatology is a new approach to investigation of glaucoma.
Posterior to the nailbed and just anterior to the proximal nailfold is the cuticle, which has no structural elements visible to the naked eye. NFC is a non-invasive imaging modality that provides a highly magnified view of the capillaries at the nailfold of digits. It has also been used in ophthalmology to show morphological changes at the nailfold capillaries of POAG and XFG/XFS patients, helping to confirm the systemic nature of these diseases.
With nailfold capillaroscopy, an extensive array of capillaries can be seen greatly enlarged on a monitor screen. Capillary loops can be imaged, stored, recorded with videoscopy, and blood flow actively imaged and measured..
The first series of papers on glaucoma were written by Prof Josef Flammer’s group at the turn of the 21st century, looking at vasospasm, blood flow in normal-tension and high-tension glaucoma, and relating ocular blood flow alterations to systemic vascular regulation and relating laser Doppler flowmetry to NFC.
Studies from Korea later associated nailbed hemorrhages and loss of nailbed capillaries to the presence of optic disc hemorrhages and investigated correlation of of heart rate variability with visual field defects and nailfold capillaroscopy.
Studies by our group began with the publication in 2015 of a paper by Pasquale et al (Nailfold Capillary Abnormalities in Primary Open-Angle Glaucoma: A Multisite Study. IOVS;56:7021) using NFC video microscopy, associating dilated capillaries, avascular zones, and hemorrhages with primary open-angle glaucoma. Successive manuscripts and presentations at conferences have indicated differences between capillary loop patterns in high-tension and normal-tension POAG and exfoliation syndrome/exfoliation glaucoma.
Our goal in this paper was to compare nailfold peripheral blood flow in XFG, which had not previously been compared to control subjects using NFC. We explored the peripheral blood flow at the nailfold of patients with high-tension glaucoma, normal-tension glaucoma, exfoliation glaucoma (XFG) and compared it to control subjects further evaluate the possible differences between these glaucoma entities. We examined the morphology and extent of nailfold capillary loops, vascular tortuosity, blood flow, and nailfold hemorrhages. (more…)
Author Interviews, Cannabis, Ophthalmology / 21.12.2018
Glaucoma: CBD (cannabidiol) May Raise Pressure in Eye
There is a real possibility that CBD elevates ocular pressure and therefore the risk of glaucoma as a side-effect...
Author Interviews, Ophthalmology, UCLA / 10.10.2016
Results of the 2-Year Ocriplasmin for Treatment for Symptomatic Vitreomacular Adhesion Including Macular Hole (OASIS) Randomized Trial
MedicalResearch.com Interview with:
Pravin U. Dugel, MD
Retina Consultants of Arizona
Phoenix, Arizona; USC Roski Eye Institute
Keck School of Medicine
University of Southern California
Los Angeles, California
MedicalResearch.com: What is the background for this study?
Response: OASIS is an acronym for “OcriplASmIn for Treatment for Symptomatic Vitreomacular Adhesion including Macular Hole”. It was a Phase IIIB, randomized, prospective, sham-controlled, double-masked, multicenter clinical study. The goal of the study was to further evaluate the long-term (24 months) efficacy and safety of a single injection of 0.125mg of ocriplasmin in patients with symptomatic vitreomacular adhesion (VMA) and vitreomacular traction (VMT), including macular hole (MH).
OASIS evaluated 220 patients with symptomatic VMA/VMT. One hundred forty-six patients received ocriplasmin while 74 served as a sham control group. In the latter group, no intravitreal injection was administered. (more…)
Author Interviews, Ophthalmology / 13.09.2016
90% of Americans Live Within Short Driving Distance To Eye Care
MedicalResearch.com Interview with:
Cecilia S. Lee, MD
Department of Ophthalmology
University of Washington School of Medicine
Seattle, WA
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Access to eye care is a critical issue currently in the United States. With the expected increase in the aging US population, many eye diseases are age-related and there is an expected associated increase in demand for eye care. Prior studies have estimated access to care in many different ways including looking at providers per zipcode, utilization of billing codes, and distance to provider. We sought to estimate the access to eye care providers using a much more accurate way to estimate the driving distance to provider. Specifically, we recreated a driving route system similar to Google Maps or Apple Maps for navigation to plot direct driving routes.
(more…)
Author Interviews, Diabetes, JAMA, Ophthalmology, Telemedicine / 23.12.2015
Teleretinal Screening Can Reduce Blindness and Costs in Diabetic Eye Disease
MedicalResearch.com Interview with:
Christina Y. Weng, MD, MBA
Assistant Professor-Vitreoretinal Diseases & Surgery
Baylor College of Medicine-Cullen Eye Institute
Medical Research: What is the background for this study? What are the main findings?
Dr. Weng: Telemedicine has been around for a long time, but only recently have technological advances solidified its utility as a reliable, effective, and cost-efficient method of healthcare provision. The application of telemedicine in the field of ophthalmology has been propelled by the development of high-quality non-mydriatic cameras, HIPAA-compliant servers for the storage and transfer of patient data, and the growing demand for ophthalmological care despite the relatively stagnant supply of eye care specialists. The global epidemic of diabetes mellitus has contributed significantly to this growing demand, as the majority of patients with diabetes will develop diabetic retinopathy in their lifetime.
Today, there are over 29 million Americans with diabetes, and diabetic retinopathy is the leading cause of blindness in working age adults in the United States. The American Academy of Ophthalmology’s and American Diabetes Association’s formal screening guidelines recommend that all diabetic patients receive an annual dilated funduscopic examination. Unfortunately, the compliance rate with this recommendation is quite dismal at an estimated 50-65%. It is even lower amongst minority populations which comprise the demographic majority of those served by the Harris Health System in Harris County, Texas, the third most populous county in the United States.
In 2013, the Harris Health System initiated a teleretinal screening program housed by eight of the district’s primary care clinics. In this system, patients with diabetes are identified by their primary care provider (PCP) during their appointments, immediately directed to receive funduscopic photographs by trained on-site personnel operating non-mydriatic cameras, and provided a follow-up recommendation (e.g., referral for in-clinic examination versus repeat imaging in 1 year) depending on the interpretation of their images. The images included in our study were interpreted via two different ways—once by the IRISTM (Intelligent Retinal Imaging Systems) proprietary auto-reader and then again by a trained ophthalmic specialist from the IRISTM reading center. The primary aim of this study was to evaluate the utility of the auto-reader by comparing its results to those of the reading center.
Data for 15,015 screened diabetic patients (30,030 eyes) were included. The sensitivity of the auto-reader in detecting severe non-proliferative diabetic retinopathy or worse, deemed sight threatening diabetic eye disease (STDED), compared to the reading center interpretation of the same images was 66.4% (95% confidence interval [CI] 62.8% - 69.9%) with a false negative rate of 2%. In a population where 15.8% of diabetics have STDED, the negative predictive value of the auto-reader was 97.8% (CI 96.8% - 98.6%).
(more…)
Author Interviews, JAMA, Ophthalmology, Telemedicine / 11.09.2014
VA Effectively Uses Telemedicine To Screen for Diabetic Eye Disease
 MedicalResearch.com Interview with:
Mary G. Lynch, MD
Professor of Ophthalmology
Atlanta Veterans Affairs Medical Center Decatur, Georgia.
Department of Ophthalmology, Emory University School of Medicine, Atlanta, Georgia
Medical Research: What are the main findings of the study?
Dr. Lynch:
MedicalResearch.com Interview with:
Mary G. Lynch, MD
Professor of Ophthalmology
Atlanta Veterans Affairs Medical Center Decatur, Georgia.
Department of Ophthalmology, Emory University School of Medicine, Atlanta, Georgia
Medical Research: What are the main findings of the study?
Dr. Lynch:
- Since 2006, the VA has been systematically using teleretinal screening of patients with diabetes to screen for retinopathy in the Primary Care Clinics. Under this program, 90% of veterans with diabetes are evaluated on a regular basis. A number of patients who are screened have findings that warrant a face-to-face ophthalmic exam. No information exists on the effect of such a program on medical center resources.
- 1,935 patients underwent teleretinal screening through the Atlanta VA over a 6 month period. We reviewed the charts of the 465 (24%) of the patients who were referred for a face to face exam in the Eye Clinic.
- Data was collected for these patients to determine the reasons for referral, the accuracy of the teleretinal interpretation, the resources needed in the Eye Clinic of the Medical Center to evaluate and care for the referred patients over a two year period and possible barriers to patient care.
- Of the 465 patients referred for an exam, 260 (55.9%) actually came in for an exam. Community notes were available for an additional 66 patients. Information was available for 326 (70.1%) of the referred patients.
- The most common referring diagnoses were nonmacular diabetic retinopathy (43.2% of referrals), nerve related issues (30.8%), lens or media opacity (19.1%), age-related macular degeneration (12.9%) and diabetic macular edema (5.6%).
- 16.9% of the referred patients had 2 or more concurrent problems that put them at high risk for visual loss.
- The percentage agreement between teleretinal screening and the ophthalmic exam was high: 90.4%. Overall sensitivity was 73.6%. The detection of diabetic macular edema had the lowest sensitivity.
- A visually significant condition was detected for the first time through teleretinal screening for 142 of the patients examined (43.6%).
- The resource burden to care for referred patients was substantial.
- 36% of patients required 3 or more visits over the ensuing 2 year period.
- The treatment of diabetic macular edema had the highest resource use involving on average 5 clinic visits, 6 diagnostic procedures and 2 surgical procedures
- The most common non-refractive diagnostic procedures were visual fields and optical coherence tomography.
- The average cost to care for the referred patients (in Medicare dollars) in work RVUs alone was approximately $1,000 per patient. The cost to care for a patient with diabetic macular edema was $2673.36.
 MedicalResearch.com Interview with:
Helen A. Mintz-Hittner, M.D., F.A.C.S.
Alfred W. Lasher, III, Professor of Ophthalmology
Department of Ophthalmology and Visual Science
The University of Texas Health Science Center
at Houston-Medical School
Cizik Eye Clinic
Medical Research: What are the main findings of the study?
Dr. Mintz-Hittner:
MedicalResearch.com Interview with:
Helen A. Mintz-Hittner, M.D., F.A.C.S.
Alfred W. Lasher, III, Professor of Ophthalmology
Department of Ophthalmology and Visual Science
The University of Texas Health Science Center
at Houston-Medical School
Cizik Eye Clinic
Medical Research: What are the main findings of the study?
Dr. Mintz-Hittner:
- For retinopathy of prematurity (ROP), at age 2 ½ years, intravitreal bevacizumab (IVB) injections cause less myopia (nearsightedness) in diopters (D) compared to conventional laser therapy (CLT):f
- or Zone I: -1.51 D versus -8.44 D (7 diopters difference: p = 0.001. for Posterior Zone II: -0.58 D versus -5.83 D (5 diopters difference: p = 0.001.
Author Interviews, Ophthalmology, Stem Cells, Transplantation / 17.07.2014
Study Uses Dental Stem Cells To Promote Retinal Regeneration After Eye Injury
 MedicalResearch.com Interview with:
Ben Mead
Molecular Neuroscience Group
Neurotrauma and Neurodegeneration Section
School of Clinical and Experimental Medicine
University of Birmingham, Birmingham
Medical Research: What are the main findings of the study?
Answer: Traumatic and neurodegenerative disease of the retina lead to an irreversible loss of retinal ganglion cells (RGC) which are the neuronal cells located in the inner retina that transmit visual signals to the brain. Thus RGC injury results in visual defects which can ultimately progress into permanent blindness. One promising therapeutic approach is the use of stem cells as a source of replacement for lost retinal cells. However a theory has emerged suggesting that stem cells can act through the secretion of signalling molecules (growth factors). One stem cell that has recently shown great promise for neuronal repair are dental pulp stem cells (DPSC), which are multipotent stem cells easily isolated from adult teeth, including third molars (Mead et al 2013, 2014).
In our research, we transplanted either dental pulp stem cells or the more widely studied bone marrow-derived mesenchymal stem cell (BMSC) into the vitreous chamber of the eye after optic nerve crush (Mead et al 2013). The main finding of this study was that DPSC, to a significantly greater degree than BMSC, promoted the survival of injured RGC and the regeneration of their axons. We also showed that the mechanism of action was not through differentiation and replacement of cells but was actually paracrine mediated, i.e. through DPSC-derived growth factors (Mead et al, 2013, 2014).
(more…)
MedicalResearch.com Interview with:
Ben Mead
Molecular Neuroscience Group
Neurotrauma and Neurodegeneration Section
School of Clinical and Experimental Medicine
University of Birmingham, Birmingham
Medical Research: What are the main findings of the study?
Answer: Traumatic and neurodegenerative disease of the retina lead to an irreversible loss of retinal ganglion cells (RGC) which are the neuronal cells located in the inner retina that transmit visual signals to the brain. Thus RGC injury results in visual defects which can ultimately progress into permanent blindness. One promising therapeutic approach is the use of stem cells as a source of replacement for lost retinal cells. However a theory has emerged suggesting that stem cells can act through the secretion of signalling molecules (growth factors). One stem cell that has recently shown great promise for neuronal repair are dental pulp stem cells (DPSC), which are multipotent stem cells easily isolated from adult teeth, including third molars (Mead et al 2013, 2014).
In our research, we transplanted either dental pulp stem cells or the more widely studied bone marrow-derived mesenchymal stem cell (BMSC) into the vitreous chamber of the eye after optic nerve crush (Mead et al 2013). The main finding of this study was that DPSC, to a significantly greater degree than BMSC, promoted the survival of injured RGC and the regeneration of their axons. We also showed that the mechanism of action was not through differentiation and replacement of cells but was actually paracrine mediated, i.e. through DPSC-derived growth factors (Mead et al, 2013, 2014).
(more…)