Effect of Antibiotics During Pregnancy on Neonatal Sepsis and Mortality
Single Dose of Antibiotic Can Cut Maternal Sepsis by Half
 William A. Petri, MD PhD
Wade Hampton Frost Professor of Medicine and
Vice Chair for Research of the Department of Medicine
Professor of Medicine, Microbiology, Immunology and Cancer Biology, and Pathology,
Medicine: Infectious Diseases and International Health,
Medicine: Infectious Diseases and International Health
William A. Petri, MD PhD
Wade Hampton Frost Professor of Medicine and
Vice Chair for Research of the Department of Medicine
Professor of Medicine, Microbiology, Immunology and Cancer Biology, and Pathology,
Medicine: Infectious Diseases and International Health,
Medicine: Infectious Diseases and International HealthNew Test Aims for Early Detection of Sepsis Utilizing Coagulation Factors
CMS Mandated Sepsis Scoring Resulted in More Testing But No Change in Outcomes
Karius Test Can Detect Blood Stream Infections Before Symptoms in High Risk Patients
 Dr. Asim Ahmed MD
co-author of the study
Senior medical director at Karius
MedicalResearch.com: What is the background for this study? Would you briefly explain the basis of the Karius Test?
Response: The Karius Test is a non-invasive blood test that uses next-generation sequencing of microbial cell-free DNA to rapidly detect over 1,400 bacteria, DNA viruses, fungi, and other pathogens. Doctors primarily use the test to detect specific causative pathogens, complicated pneumonia, cardiovascular infections, and infections in immunocompromised hosts.
The Karius Test is transforming how doctors diagnose infectious diseases by helping doctors identify the precise pathogens infecting patients.
The Karius Test offers a higher diagnostic yield and faster time-to-diagnosis than conventional tests - with the potential to eliminate invasive diagnostic procedures like biopsies.
(more…)
Dr. Asim Ahmed MD
co-author of the study
Senior medical director at Karius
MedicalResearch.com: What is the background for this study? Would you briefly explain the basis of the Karius Test?
Response: The Karius Test is a non-invasive blood test that uses next-generation sequencing of microbial cell-free DNA to rapidly detect over 1,400 bacteria, DNA viruses, fungi, and other pathogens. Doctors primarily use the test to detect specific causative pathogens, complicated pneumonia, cardiovascular infections, and infections in immunocompromised hosts.
The Karius Test is transforming how doctors diagnose infectious diseases by helping doctors identify the precise pathogens infecting patients.
The Karius Test offers a higher diagnostic yield and faster time-to-diagnosis than conventional tests - with the potential to eliminate invasive diagnostic procedures like biopsies.
(more…)Does PCSK9 Genetic Variation Help Predict Risk of Sepsis?
T2Bacteria Panel Can Detect Blood Stream Infections in Hours, not Days
Most Deaths From Sepsis Occur in Frail Older Adults and Are Not Preventable
Steroids Associated With Reduced Mortality in Adults with Sepsis
Use of IV Fluids by EMTs Reduced Morality in Septic Patients With Low Blood Pressure
MedicalResearch.com Interview with: Daniel J. Lane PhD
Daniel J. Lane PhD
Institute of Health Policy, Management and Evaluation
Dalla Lana School of Public Health, University of Toronto
Rescu, Li Ka Shing Knowledge Institute, St Michael’s Hospital
Toronto, Ontario, Canada
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Early resuscitation and early antibiotics have become the mainstay treatment for patients with sepsis. The time to initiation of these treatments is thought to be an important factor in patients surviving their disease; however, the independent benefits or harms of intravenous fluid resuscitation, in particular a more aggressive versus more conservative approach to this therapy, remains difficult to evaluate given the concurrent use of these therapies in hospital.
To gain a better understanding of this treatment independent of antibiotic use, we assessed intravenous fluid resuscitation by paramedics on the in-hospital mortality of patients with sepsis. By accounting for the interaction between initial systolic blood pressure and the treatment, we found that earlier resuscitation by paramedics was associated with decreased mortality in patients with low initial blood pressures but not associated with mortality for patients with normal or higher initial blood pressures.
“Rory’s Regulations” Improves Pediatric Sepsis Care
New Cephalosporin Combination Tested for Complicated Sepsis Patients
Merck Tests New Antibiotic Combination For Hard to Treat Bacterial Infections
Hospital Onset Clostridium difficile Infections Increased With Electronic Sepsis Alerts
Incidence of Sepsis Stable, But Mortality Remains High
Rory’s Regulations: Faster Is Better When It Comes To Sepsis Care
EHRs Can Facilitate Rapid Detection and Treatment of Sepsis
How Does Emergency Room Crowding Affect Care of Septic Patients?
Sepsis Linked To High Rate of Hospital Readmissions
Elevated Lactate Linked To Increased Mortality in Children With Sepsis
Survivors of Sepsis Require Complicated, Coordinated Follow-Up Care
Point of Care Platform Aims To Detect Sepsis in 90 Minutes
Electronic Alerts Improved Sepsis Care and Outcomes
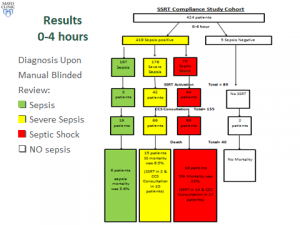 Two blinded reviewers retrospectively abstracted data on clinical trajectory and outcomes of all patients with sepsis and SS/S admitted at a single academic medical center between September 2013 and September 2014. Given importance of timely recognition and interventions in S/SS, we specifically focused on 2 periods: 0-4 hours and 4-12 hours after hospital admission. Additionally, we compared the compliance to “standard of care” between the SSRT pre-implementation period and the study period.
There were 167 patients admitted with sepsis, among which there were 3 SSRT activations and sepsis mortality was 3.6%. There were 176 patients with SS, SSRT was called in 42 (23%) and SS mortality was 8.5%. CCS was involved in 66 patients and mortality was 6.9% if SSRT was activated, versus 21.6% if SSRT was not activated. There were 76 patients with septic shock, SSRT was called in 44 (57%) and septic shock mortality was 25%. Critical Care Service (CCS) was involved in 68 patients and mortality rates with and without SSRT were 30.9% and 15.4%, respectively. The all-or-none compliance with applicable goals of resuscitation improved from the baseline 0% to over 50% at the study period end. Overall observed/expected sepsis mortality index improved from 1.38 pre-SSRT to 0.68 post-SSRT implementation.
(more…)
Two blinded reviewers retrospectively abstracted data on clinical trajectory and outcomes of all patients with sepsis and SS/S admitted at a single academic medical center between September 2013 and September 2014. Given importance of timely recognition and interventions in S/SS, we specifically focused on 2 periods: 0-4 hours and 4-12 hours after hospital admission. Additionally, we compared the compliance to “standard of care” between the SSRT pre-implementation period and the study period.
There were 167 patients admitted with sepsis, among which there were 3 SSRT activations and sepsis mortality was 3.6%. There were 176 patients with SS, SSRT was called in 42 (23%) and SS mortality was 8.5%. CCS was involved in 66 patients and mortality was 6.9% if SSRT was activated, versus 21.6% if SSRT was not activated. There were 76 patients with septic shock, SSRT was called in 44 (57%) and septic shock mortality was 25%. Critical Care Service (CCS) was involved in 68 patients and mortality rates with and without SSRT were 30.9% and 15.4%, respectively. The all-or-none compliance with applicable goals of resuscitation improved from the baseline 0% to over 50% at the study period end. Overall observed/expected sepsis mortality index improved from 1.38 pre-SSRT to 0.68 post-SSRT implementation.
(more…)Personalized Risk Calculations May Reduce Readmissions Of Sepsis Survivors
 MedicalResearch.com Interview with:
Hallie Prescott, MD, MSc
Clinical Lecturer, Internal Medicine
Division of Pulmonary & Critical Care Medicine
University of Michigan Health System
Ann Arbor, MI 48109-2800
Medical Research: What is the background for this study? What are the main findings?
Dr. Prescott: The post-hospital period has been widely recognized as a vulnerable time for patients. In particular, patients who survive sepsis are frequently readmitted to the hospital in the following three months.
In this study, we examined data from 2,600 survivors of sepsis, a severe infection that leads to organ failure. About 42% of the sepsis patients were readmitted in the next 90 days, similar to the rate seen for patients hospitalized for other acute conditions.
However, the reasons for hospital readmission after sepsis are different. A greater number of patients are re-hospitalized for “ambulatory-care sensitive conditions”, which are conditions that could potentially be prevented or treated early in the outpatient setting to avoid a hospital stay.
(more…)
MedicalResearch.com Interview with:
Hallie Prescott, MD, MSc
Clinical Lecturer, Internal Medicine
Division of Pulmonary & Critical Care Medicine
University of Michigan Health System
Ann Arbor, MI 48109-2800
Medical Research: What is the background for this study? What are the main findings?
Dr. Prescott: The post-hospital period has been widely recognized as a vulnerable time for patients. In particular, patients who survive sepsis are frequently readmitted to the hospital in the following three months.
In this study, we examined data from 2,600 survivors of sepsis, a severe infection that leads to organ failure. About 42% of the sepsis patients were readmitted in the next 90 days, similar to the rate seen for patients hospitalized for other acute conditions.
However, the reasons for hospital readmission after sepsis are different. A greater number of patients are re-hospitalized for “ambulatory-care sensitive conditions”, which are conditions that could potentially be prevented or treated early in the outpatient setting to avoid a hospital stay.
(more…)Burn Patients: White Blood Cell Motility Predictive of Sepsis
 MedicalResearch.com Interview with:
Daniel Irimia, M.D., Ph.D.
Assistant Professor
Division of Surgery, Science & Bioengineering
Massachusetts General Hospital and Harvard Medical School
Associate Director, BioMEMS Resource Center
Boston, MA 02129
Medical Research: What is the background for this study? What are the main findings?
Response: Sepsis is affecting more than half of the patients with major burn injuries (20 percent of body surface) and is the leading cause of death among these patients. Sepsis is also a significant complication for other critically ill patients. More than one million Americans are affected and it has been estimated that approximately 30% of these people die, despite significant advances in life support and antibiotics. Early diagnosis is essential, and it has been calculated that every 6 hours of delay in a sepsis diagnosis decreases the chances of survival by 10 percent.
We have found that the motility of the white blood cells called neutrophils, inside a microfluidic device, is significantly altered two to three days before sepsis develops. (more…)
MedicalResearch.com Interview with:
Daniel Irimia, M.D., Ph.D.
Assistant Professor
Division of Surgery, Science & Bioengineering
Massachusetts General Hospital and Harvard Medical School
Associate Director, BioMEMS Resource Center
Boston, MA 02129
Medical Research: What is the background for this study? What are the main findings?
Response: Sepsis is affecting more than half of the patients with major burn injuries (20 percent of body surface) and is the leading cause of death among these patients. Sepsis is also a significant complication for other critically ill patients. More than one million Americans are affected and it has been estimated that approximately 30% of these people die, despite significant advances in life support and antibiotics. Early diagnosis is essential, and it has been calculated that every 6 hours of delay in a sepsis diagnosis decreases the chances of survival by 10 percent.
We have found that the motility of the white blood cells called neutrophils, inside a microfluidic device, is significantly altered two to three days before sepsis develops. (more…)Septic Shock Patients Often Require Hospital Readmission
 MedicalResearch.com Interview with:
Mark E Mikkelsen, MD, MSCE
Assistant Professor of Medicine
Hospital of the University of Pennsylvania
Medical Research: What is the background for this study? What are the main findings?
Dr. Mikkelsen: Sepsis is common, afflicting as many as 3 million Americans each year. It is also costly, both in terms of health care expenditures that exceed $20 billion for acute care and in terms of the impact it has on patients and their families. To date, studies have focused on what happens to septic shock patients during the initial hospitalization. However, because more patients are surviving sepsis than ever, we sought to examine the enduring impact of septic shock post-discharge. We focused on the first 30 days after discharge and asked several simple questions. First, how often did patients require re-hospitalization after septic shock? And second, why were patients re-hospitalized?
We found that 23% of septic shock survivors were re-hospitalized within 30 days, many of them within 2 weeks. A life-threatening condition such as recurrent infection was the reason for readmission and 16% of readmissions resulted in death or a transition to hospice.
(more…)
MedicalResearch.com Interview with:
Mark E Mikkelsen, MD, MSCE
Assistant Professor of Medicine
Hospital of the University of Pennsylvania
Medical Research: What is the background for this study? What are the main findings?
Dr. Mikkelsen: Sepsis is common, afflicting as many as 3 million Americans each year. It is also costly, both in terms of health care expenditures that exceed $20 billion for acute care and in terms of the impact it has on patients and their families. To date, studies have focused on what happens to septic shock patients during the initial hospitalization. However, because more patients are surviving sepsis than ever, we sought to examine the enduring impact of septic shock post-discharge. We focused on the first 30 days after discharge and asked several simple questions. First, how often did patients require re-hospitalization after septic shock? And second, why were patients re-hospitalized?
We found that 23% of septic shock survivors were re-hospitalized within 30 days, many of them within 2 weeks. A life-threatening condition such as recurrent infection was the reason for readmission and 16% of readmissions resulted in death or a transition to hospice.
(more…)Genetic Signature Provides Early Prediction of Sepsis and Organ Failure
 MedicalResearch.com Interview with:
Dr R.E.W. (Bob) Hancock, OC, OBC, FRSC
{Canada Research Chair and Professor, Department of Microbiology and Immunology,UBC}
Director, Centre for Microbial Diseases and Immunity Research
University of British Columbia,
Vancouver, British Columbia, Canada
MedicalResearch: What is the background for this study? What are the main findings?
Dr. Hancock: We wanted to understand how patients transitioned from the hyperinflammatory phase (cytokine storm) of sepsis to the hypoinflammatory (immunosuppressive) phase of sepsis (inability to respond appropriately to infections). About 15% of patients die in this first phase and 20% in the second phase, making sepsis one of the most deadly syndromes (35% overall mortality, 5 million deaths [8.3% of all deaths] annually worldwide). We hypothesized that immunosuppression was characterized by a state termed endotoxin tolerance a cellular amnesia (termed cellular reprogramming) in which cells fail to respond to microbial cues.
Overall we found that an Endotoxin Tolerance gene signature is significantly associated with the subsequent development of confirmed sepsis and new organ dysfunction in patients who had suspected sepsis. All 620 sepsis patients in retrospective and new analyses presented with an expression profile strongly associated with the endotoxin tolerance signature (p<0.01; AUC 96.1%). This occurred in fact very early in sepsis and in a new clinical study we found that the signature could be detected already in the emergency ward at first clinical presentation and 24-48 hours prior to definitive diagnosis. Importantly, this signature further differentiated between suspected sepsis patients who did, or did not, go on to develop confirmed sepsis, and predicted the development of organ dysfunction.
(more…)
MedicalResearch.com Interview with:
Dr R.E.W. (Bob) Hancock, OC, OBC, FRSC
{Canada Research Chair and Professor, Department of Microbiology and Immunology,UBC}
Director, Centre for Microbial Diseases and Immunity Research
University of British Columbia,
Vancouver, British Columbia, Canada
MedicalResearch: What is the background for this study? What are the main findings?
Dr. Hancock: We wanted to understand how patients transitioned from the hyperinflammatory phase (cytokine storm) of sepsis to the hypoinflammatory (immunosuppressive) phase of sepsis (inability to respond appropriately to infections). About 15% of patients die in this first phase and 20% in the second phase, making sepsis one of the most deadly syndromes (35% overall mortality, 5 million deaths [8.3% of all deaths] annually worldwide). We hypothesized that immunosuppression was characterized by a state termed endotoxin tolerance a cellular amnesia (termed cellular reprogramming) in which cells fail to respond to microbial cues.
Overall we found that an Endotoxin Tolerance gene signature is significantly associated with the subsequent development of confirmed sepsis and new organ dysfunction in patients who had suspected sepsis. All 620 sepsis patients in retrospective and new analyses presented with an expression profile strongly associated with the endotoxin tolerance signature (p<0.01; AUC 96.1%). This occurred in fact very early in sepsis and in a new clinical study we found that the signature could be detected already in the emergency ward at first clinical presentation and 24-48 hours prior to definitive diagnosis. Importantly, this signature further differentiated between suspected sepsis patients who did, or did not, go on to develop confirmed sepsis, and predicted the development of organ dysfunction.
(more…)Sepsis-Sniffer Tool Better Identifies Patients Requiring Advance Care
 MedicalResearch.com Interview with:
Craig A Umscheid, MD, MSCE, FACP
Assistant Professor of Medicine and Epidemiology
Director, Center for Evidence-based Practice
Medical Director, Clinical Decision Support
Chair, Department of Medicine Quality Committee
Senior Associate Director, ECRI-Penn AHRQ Evidence-based Practice Center, University of Pennsylvania Philadelphia, PA 19104
Medical Research: What are the main findings of the study?
Dr. Umscheid: We developed an automated early warning and response system for sepsis that has resulted in a marked increase in sepsis identification and care, transfer to the ICU, and an indication of fewer deaths due to sepsis.
Sepsis is a potentially life-threatening complication of an infection; it can severely impair the body’s organs, causing them to fail. There are as many as three million cases of severe sepsis and 750,000 resulting deaths in the United States annually. Early detection and treatment, typically with antibiotics and intravenous fluids, is critical for survival.
The Penn prediction tool, dubbed the “sepsis sniffer,” uses laboratory and vital-sign data (such as body temperature, heart rate, and blood pressure) in the electronic health record of hospital inpatients to identify those at risk for sepsis. When certain data thresholds are detected, the system automatically sends an electronic communication to physicians, nurses, and other members of a rapid response team who quickly perform a bedside evaluation and take action to stabilize or transfer the patient to the intensive care unit if warranted.
We developed the prediction tool using 4,575 patients admitted to the University of Pennsylvania Health System (UPHS) in October 2011. We then validated the tool during a pre-implementation period from June to September 2012, when data on admitted patients was evaluated and alerts triggered in a database, but no notifications were sent to providers on the ground. Outcomes in that control period were then compared to a post-implementation period from June to September 2013. The total number of patients included in the pre and post periods was 31,093.
(more…)
MedicalResearch.com Interview with:
Craig A Umscheid, MD, MSCE, FACP
Assistant Professor of Medicine and Epidemiology
Director, Center for Evidence-based Practice
Medical Director, Clinical Decision Support
Chair, Department of Medicine Quality Committee
Senior Associate Director, ECRI-Penn AHRQ Evidence-based Practice Center, University of Pennsylvania Philadelphia, PA 19104
Medical Research: What are the main findings of the study?
Dr. Umscheid: We developed an automated early warning and response system for sepsis that has resulted in a marked increase in sepsis identification and care, transfer to the ICU, and an indication of fewer deaths due to sepsis.
Sepsis is a potentially life-threatening complication of an infection; it can severely impair the body’s organs, causing them to fail. There are as many as three million cases of severe sepsis and 750,000 resulting deaths in the United States annually. Early detection and treatment, typically with antibiotics and intravenous fluids, is critical for survival.
The Penn prediction tool, dubbed the “sepsis sniffer,” uses laboratory and vital-sign data (such as body temperature, heart rate, and blood pressure) in the electronic health record of hospital inpatients to identify those at risk for sepsis. When certain data thresholds are detected, the system automatically sends an electronic communication to physicians, nurses, and other members of a rapid response team who quickly perform a bedside evaluation and take action to stabilize or transfer the patient to the intensive care unit if warranted.
We developed the prediction tool using 4,575 patients admitted to the University of Pennsylvania Health System (UPHS) in October 2011. We then validated the tool during a pre-implementation period from June to September 2012, when data on admitted patients was evaluated and alerts triggered in a database, but no notifications were sent to providers on the ground. Outcomes in that control period were then compared to a post-implementation period from June to September 2013. The total number of patients included in the pre and post periods was 31,093.
(more…)- 1
- 2









