MedicalResearch.com Interview with:
Dr Pam Sonnenberg
Reader in Infectious Disease Epidemiology
Research Department of Infection & Population Health
University College London
London
MedicalResearch: What is the background for this study? What are the main findings?
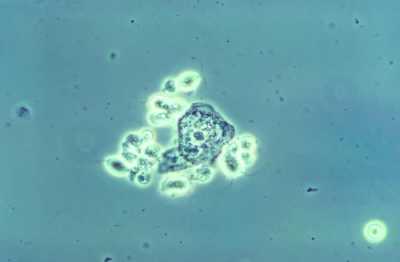
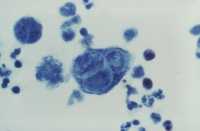
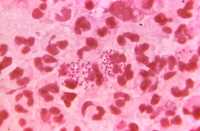
Dr. Sonnenberg: This study strengthens growing evidence that
Mycoplasma genitalium (MG) is a sexually transmitted infection (STI). Analyses of over 4500 of urine samples from Britain’s third National Survey of Sexual Attitudes and Lifestyles (Natsal-3) showed that MG was prevalent in up to 1% of the general population aged 16-44, who had reported at least one sexual partner. Prevalence was much higher in those who had reported more than four sexual partners in the past year – 5.2% in men and 3.1% in women. Absence of the infection in over 200 16-17 year olds who had not had vaginal, anal, or oral sex provided further evidence that MG is transmitted sexually. The study also analysed risk factors for
Mycoplasma genitalium, such as ethnicity, number of partners, and areas of deprivation. There were strong associations with risky sexual behaviours, with similar behavioural risk factors to other known STIs. The authors found that men of Black ethnicity and those living in the most deprived areas were more likely to test positive for MG. Over 90% of
Mycoplasma genitalium in men and over two-thirds of MG cases in women were in those aged 25–44 years; an age group who would not be included in STI prevention measures currently aimed at young people in Britain. Interestingly, the majority of participants who tested positive for MG did not report any STI symptoms in the last month. Over half of women did not report any symptoms, but among those who did, bleeding after sex was most common. Over 90% of MG positive men did not report any symptoms.
(more…)