Author Interviews, Breast Cancer, Cancer Research, Genetic Research, Ovarian Cancer / 22.07.2020
Population Based BRCA-Testing Can Detect More Breast and Ovarian Cancers, and Be Cost-Effective
MedicalResearch.com Interview with:
Prof Ranjit Manchanda MD, MRCOG, PhD
Professor of Gynaecological Oncology & Consultant Gynaecological Oncologist
NHS Innovation Accelerator (NIA) Fellow
Integrated Academic Training Programme Director
London Specialty School of Obstetrics & Gynaecology, Health Education England
Specialty Research Lead for Gynaecological Cancer, NIHR, North Thames Clinical Research Network
Cancer Research UK, Barts Centre | Queen Mary University of London
Centre for Cancer Prevention, Wolfson Institute of Preventive Medicine | Charterhouse Square | London
Department of Gynaecological Oncology | Barts Health NHS Trust, Royal London Hospital
MedicalResearch.com: What is the background for this study?
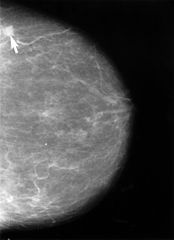
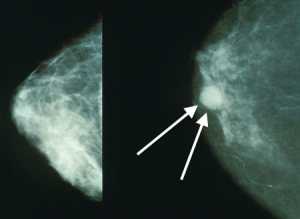
Response: Around 10–20% of ovarian cancers and 6% breast cancers overall are caused by inheritable BRCA1/BRCA2 mutations. Women carrying BRCA1/BRCA2 mutations have a 17–44% risk of ovarian cancer and 69–72% risk of breast cancer until age 80 years. Most of these cancers can be prevented in unaffected BRCA1/BRCA2 women carriers. Women can opt for a range of options including screening, preventive, and reproductive choices to minimise their risk.
The current approach uses established clinical-criteria/family-history (FH) based a priori BRCA probability thresholds to identify high-risk individuals eligible for BRCA testing. However, this requires individuals and health practitioners to recognise and act on a significant FH. BRCA carriers, who are unaware of their FH, unappreciative of its risk/significance, not proactive in seeking advice, or lack a strong FH (small families/paternal inheritance/chance) get excluded. Over 50% BRCA carriers do not fulfil clinical criteria and are missed.
Despite >25 years of BRCA testing and effective mechanisms for prevention, current guidelines and access to testing pathways remain complex and associated with a massive under-utilisation of genetic testing. Only 20% of eligible women have accessed/undergone genetic testing and our earlier analysis showed that 97% of BRCA carriers in the population remain unidentified. Current detection rates are inadequate to identify all BRCA carriers and even doubling detection rates will not work.
Why should we wait for decades for people to develop cancer before identifying BRCA carriers and unaffected at-risk family members to offer prevention?. This highlights substantial missed opportunities for early detection and prevention. A new population testing approach can change this. Jewish population studies show this is feasible, acceptable, has high satisfaction (91–95%), significantly reduces anxiety, doesn’t harm psychological well-being or quality of life, and is extremely cost-effective. However, this has not been evaluated in the general population and in particular across different countries or health systems. The potential applicability and scope for this approach transcends continents and countries. Additionally, for interventions to be sustainable, they need to be cost-effective and affordable.
We have undertaken a cost-effectiveness analysis of population based BRCA testing compared with current standard clinical testing of women designated as high risk, across high income countries (UK/USA/Netherlands), upper-middle income countries (China/Brazil), and low-middle income country (India).
(more…)