Author Interviews, Clots - Coagulation, NEJM / 12.08.2020
NEJM: Compression Therapy Prevention of Recurrent Cellulitis Without Antibiotics
MedicalResearch.com Interview with:
Elizabeth Webb, M.P.H
Physiotherapy Department
Calvary Public Hospital Bruce
Bruce, Australia
MedicalResearch.com: What is the background for this study?
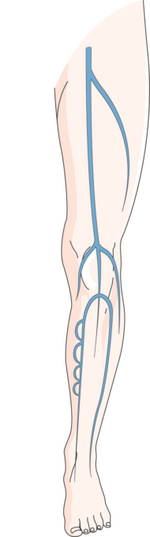
Response: Our study showed that in patients with a history of leg swelling (chronic edema), compression therapy by a skilled lymphedema therapist reduced the risk of infection in the leg (cellulitis) by a huge 77%. With up to 47% of patients experiencing recurrence of cellulitis in their legs within 3 years, this result is a game-changer in terms of our approach to managing patients with leg swelling and recurrent cellulitis.
Until now, the use of prophylactic antibiotics to prevent cellulitis has been the only evidence-based practice. We know however, there are many reasons why avoidance of antibiotics is important within our community. (more…)