MedicalResearch.com Interview with:
Paul Burton, MD, PhD, FACC
Vice President, Medical Affairs
Janssen
MedicalResearch.com: What is the background for this study? What are the main findings?
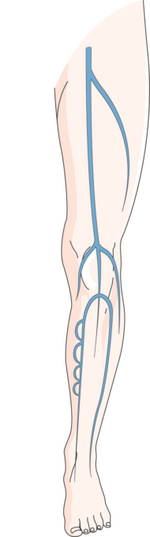
Response: Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), affects more than 900,000 Americans each year; one-third of these occurrences are fatal. Once a person experiences a VTE, they are at risk of having another occurrence. Guidelines currently recommend anticoagulant therapy with a non-vitamin K antagonist oral anticoagulant (NOAC), like XARELTO
® (rivaroxaban), for three months or longer. Once anticoagulant therapy is stopped, up to 10 percent of people will experience a recurrence during the first year and up to 20 percent within three years. In people who decide to stop anticoagulant therapy, guidelines currently suggest using aspirin for long-term prevention of recurrent VTE rather than no aspirin at all.
The Phase 3 EINSTEIN CHOICE study was designed to compare the efficacy and safety of XARELTO
® to aspirin for continued VTE management in people who experienced an initial VTE. The study met its primary endpoint, finding both XARELTO
® doses (10 mg or 20 mg once daily) to be superior to aspirin 100 mg once daily in preventing recurrent VTE, with no significant impact on safety. Specifically, XARELTO
® 10 mg reduced the risk of recurrent VTE by 74 percent and XARELTO
® 20 mg by 66 percent. Rates of major bleeding were comparable and low across all treatment groups.
These results were presented at the American College of Cardiology's 64th Annual Scientific Session (ACC.17) during a Joint ACC/
Journal of American Medical Association Late-Breaking Clinical Trials
session and published simultaneously in
The New England Journal of Medicine.
(more…)