Own a dog? Then your vet must have shared a thing or two about the risks of ticks and even warned you about Lyme disease.
But is your furry friend only at risk of this bacterial infection? You’re wrong if you think so. Humans can also get Lyme disease if a black-legged tick carrying the borrelia bacteria bites them.
Just recently, the comedian and actress Miranda Hart opened up about how she struggled with chronic fatigue syndrome after she was diagnosed with Lyme disease.
Many other famous people say they have been struck by this tick-borne bacterial infection. Those include Real Housewives of Beverly Hills star Yolanda Hadid and her daughter, model Bella Hadid, comic Amy Schumer, actor Ben Stiller, and singer Justin Bieber.
As high-profile names share their struggles, awareness of Lyme is spreading fast. But so are the myths. So, let’s separate the facts from the fiction surrounding this disease.
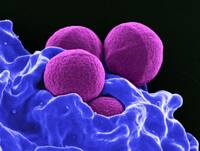
Author Interviews, Lancet, MRSA, NIH / 18.01.2023
Specific Probiotic Dramatically Decreases Staph Aureus in the Gut
MedicalResearch.com Interview with:
Michael Otto PhD
Senior Investigator
Laboratory of Bacteriology
Chief of the Pathogen Molecular Genetics Section
NIAID, NIH
Bethesda, MD 20814
MedicalResearch.com: What is the background for this study?
Response: Staphylococcus aureus is one the of the most important causes of infectious diseases worldwide. It is known mostly for causing skin infections in the community and as a hospital-associated pathogen. It is in fact the most frequent cause of infections patients acquire in the hospital when they are weakened by underlying diseases or immune-suppressing therapy. The type of infections Staph can cause in these situations are diverse – comprising bone, lung, and blood infections (sepsis) - and can be quite severe and often fatal.
Except for moderately severe skin infections that may not require antibiotic treatment, treatment of Staph infections is by antibiotics. S. aureus has naturally been very responsive to penicillin-type antibiotics, but already in the mid of the last century, resistance to penicillin spread worldwide. Then, methicillin was invented to overcome this resistance, but nowadays there also is considerable spread of methicillin-resistant strains (MRSA).
The current situation is difficult for two reasons:
- First, S. aureus has become increasingly resistant to many antibiotics, and
- Second, the alternatives to methicillin are often by far not as efficient as penicillin/methicillin against Staph.
AHA Journals, Author Interviews, Heart Disease, Stroke / 12.03.2021
Stroke Risk: AI Can Help Predict Who Might Develop Atrial Fibrillation
MedicalResearch.com Interview with:
Brandon K Fornwalt, MD, PhD
Associate Professor, Director Department of Imaging Science and Innovation
Geisinger
MedicalResearch.com: What is the background for this study?
Response: Atrial fibrillation (AF) is an abnormal heart rhythm that is associated with outcomes such as stroke, heart failure and death. If we know a patient has atrial fibrillation, we can treat them to reduce the risk of stroke by nearly two-thirds. Unfortunately, patients often don’t know they have AF. They present initially with a stroke, and we have no chance to treat them before this happens. If we could predict who is at high risk of either currently having AF or developing it in the near future, we could intervene earlier and hopefully reduce bad outcomes like stroke. Artificial intelligence approaches may be able to help with this task. (more…)
AHA Journals, Author Interviews, Heart Disease, Race/Ethnic Diversity, Stroke / 05.03.2021
Cultural Factors May Account for Lack of Preventive Measures in LatinX Stroke Patients
MedicalResearch.com Interview with:
Fernando D Testai, MD, PhD, FAHA
Associate Professor of Neurology and Rehabilitation
Stroke Medical Director
University of Illinois Health
MedicalResearch.com: What is the background for this study?
Response: Stroke constitutes a leading cause of disability and mortality in the United States. Large observational studies have shown that up to 90% of the strokes are caused by modifiable vascular risk factors, including hypertension, diabetes mellitus, and several others. In addition, previous history of stroke is one of the most powerful predictors of recurrent stroke. Thus, controlling vascular risk factors in patients with stroke is of paramount importance. To this end, the American Heart Association and the American Stroke Association have developed specific targets for blood pressure, glycemic, and cholesterol levels.
(more…)
Author Interviews, CDC, JAMA, Stroke, USPSTF / 11.02.2021
USPSTF: Should Asymptomatic Patients Be Screened for Coronary Artery Disease?
MedicalResearch.com Interview with:
Aaron B. Caughey, M.D., M.P.P., M.P.H., Ph.D.
Professor and Chair
Department of Obstetrics and Gynecolog
Associate dean for Women’s Health Research and Policy
Oregon Health & Science University Portland, OR.
Founder and Chair
Centers for Disease Control and Prevention–funded Oregon Perinatal Collaborative
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Stroke is a leading cause of death and disability in the United States and can be devastating to those affected. One of many risk factors for stroke is carotid artery stenosis (CAS), which is the narrowing of the arteries that run along the sides of the neck and supply blood to the brain.
The Task Force wants to help prevent people from having a stroke, but evidence shows that screening for CAS in people without symptoms does not help prevent strokes and can actually lead to harmful events such as stroke, heart attack, or death. Since the harms of screening greatly outweigh the benefits, the Task Force continues to recommend against screening for CAS among adults who do not have any signs or symptoms of a blocked artery in the neck. (more…)
AHA Journals, Author Interviews, COVID -19 Coronavirus, NYU / 21.05.2020
NYU Study Finds Strokes More Common and Severe in Younger Patients
MedicalResearch.com Interview with:
Shadi Yaghi, MD
Assistant Professor
Department of Neurology at NYU Grossman School of Medicine
Director, Clinical Vascular Neurology Research, NYU Langone Health
Director, Vascular Neurology, NYU Langone Hospital-Brooklyn
MedicalResearch.com: What is the background for this study?
Response: Our aim was to determine the characteristics of imaging proven ischemic stroke in the setting of COVID-19 infection and compare them to those of ischemic stroke but without COVID-19 infection.
(more…)
Author Interviews, COVID -19 Coronavirus, Emergency Care, Infections, NEJM, Stroke / 09.05.2020
COVID Pandemic: Number of Patients Seeking Stroke Care Plummets
MedicalResearch.com Interview with:
Akash Kansagra, MD, MS
Assistant Professor of Radiology
Neurological Surgery, and Neurology
Director, Endovascular Surgical Neuroradiology
Co-Director, Stroke and Cerebrovascular Center
Washington University and Barnes-Jewish Hospital
MedicalResearch.com: What is the background for this study?
Response: Over the past five years, medicine has made enormous strides in stroke treatment. The effectiveness of these therapies has been absolutely astounding, and our ability to get patients to hospitals that can provide this life-saving care has also improved dramatically. (more…)
AHA Journals, Author Interviews, Gender Differences, Stroke / 30.11.2019
Stroke: Sex Differences in Treatment and Outcome
MedicalResearch.com Interview with:
Cheryl Carcel MD
Research Fellow, Stroke & Women's Health Program
Conjoint Senior Lecturer, Faculty of Medicine, UNSW Sydney
Associate Lecturer, Sydney Medical School, The University of Sydney
The George Institute for Global Health | Australia
MedicalResearch.com: What is the background for this study?
Response: This study builds on previous findings of differences in the presentation, treatment and outcome for women and men who experience stroke. For this analysis, we pooled five large international, multicenter, randomized controlled trials that included the following: the Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trials (INTERACT-1 and -2 studies), the alteplase-dose arm of the Enhanced Control of Hypertension and Thrombolysis Stroke study (ENCHANTED), the Head Position in Acute Stroke Trial (HeadPoST), and the Scandinavian Candesartan Acute Stroke Trial (SCAST). (more…)
Author Interviews, Lipids, NEJM, Neurological Disorders, Stroke / 18.11.2019
Lower LDL Cholesterol Linked to Reduced Risk of Recurrent Stroke
MedicalResearch.com Interview with:
Pierre Amarenco, MD
Professor and Chairman
Paris University, Paris, France
INSERM
Department of Neurology and Stroke Centre
Bichat Hospital
Paris, France
MedicalResearch.com: What is the background for this study?
Response: The rationale of the Treat Stroke to target trial was that after we published the SPARCL trial in 2006 (atorvastatin 80 mg/day vs placebo in patients with stroke) which showed a 16% relative risk reduction of recurrent stroke, we performed several pre specified and post hoc analyses, showing that in SPARCL patients randomized with "atherosclerotic disease" the risk reduction for the primary endpoint was much higher (33%), and in in patients achieving a LDL cholesterol of less than 70 mg/dL as compared to those achieving a LDL cholesterol 100 mg/dL or higher, the risk reduction was 28%.
Therefore to confirm this findings, we designed the TST trial, which was an investigator initiated trial funded by the french ministry of health, and enrolled patients with an ischemic stroke due to atherosclerotic stenosis and randomized them to either a target LDL cholesterol of less than 70 mg/dL or a target LDL cholesterol of 90 to 110 mg/dL. To achieve these goals, the investigators could use any statin available on the market, and titrate the dosage of the statin to get to the assigned target. They could also use ezetimibe on top of statin therapy if a high dosage of statin was not sufficient to get to the target level assigned by randomization. (more…)
MedicalResearch.com Interview with:
Mwenya Mubanga, MD, PhD
Postdoctoral Researcher
Department of Medical Epidemiology and Biostatistics | Karolinska Institutet
Childhood Allergy and Asthma
Stockholm
MedicalResearch.com: What is the background for this study?
Response: In a previous study we showed that dog ownership was associated with a lower risk of composite cardiovascular death and all-cause death as compared to non-dog owners.1 In this follow-up, we assessed the hypothesis that dog ownership was associated with better survival after either an acute myocardial infarction or an ischemic stroke.
Using the rich Swedish national registers, we identified more than 300,000 adults aged 45 to 80 and linked their individual-level health records to information on socio-economic, demographic and death data. (more…)
AHA Journals, Author Interviews, Environmental Risks, Heart Disease, Stroke / 26.09.2019
High Pesticide Exposure Associated With Increased CAD and Stroke Risk
MedicalResearch.com Interview with:
Zara Berg, Ph.D
Fort Peck Community College
Poplar, Montana
MedicalResearch.com: What is the background for this study?
Response: This study is part of the cohort that consist of the Honolulu Heart Program (HHP) and what later became the Honolulu-Asia Aging study. HHP study cardiovascular research starting in the 1960’s, which is equivalent to the Framingham Study.
This study was used to establish the epidemiology parameters for cardiovascular diseases and is one of the longest longitudinal (34 years of follow-up) study on cardiovascular diseases and other diseases that effect the elderly. The participants were all Japanese that fought in WWII which is a sample size of 8,006 participants.
In additional, there is multiple studies based on this cohort for the last fifty plus years, ranging from occupational exposure, cancer, neurological diseases, and cardiovascular diseases. (more…)
Author Interviews, BMJ, Heart Disease, Red Meat, Stroke, Vegetarians / 10.09.2019
Vegetarians: Less Heart Disease, More Strokes
MedicalResearch.com Interview with:
Dr Tammy Y N Tong PhD
Cancer Epidemiology Unit
Nuffield Department of Population Health
University of Oxford, Oxford, UK
MedicalResearch.com: What is the background for this study?
Response: Vegetarian and vegan diets have become increasingly popular in recent years, partly due to the perceived health benefits, but also concerns about the environment and animal welfare. However, the full extent of the potential health benefits and hazards of these diets is not well understood. Previous studies have suggested that vegetarians have a lower risk of coronary heart disease than non-vegetarians, but data from large studies are limited, and little has been reported on the difference in risk of stroke.
(more…)
Author Interviews, Blood Pressure - Hypertension, JAMA, Stroke / 29.07.2019
RESPECT Study: Intensive Blood Pressure Control Better for Secondary Stroke Prevention
MedicalResearch.com Interview with:
 Kazuo Kitagawa, MD PhD
Department of Neurology
Tokyo Women's Medical University
Tokyo, Japan
MedicalResearch.com: What is the background for this study? What are the main findings
Response: Reduction in blood pressure (BP) reduces the rates of recurrent stroke, but the optimum BP target remained unclear.
The results of RESPECT Study together with up-dated meta-analysis showed the benefit of intensive blood pressure lowering (<130/80 mmHg) compared with standard BP lowering (<140/90 mmHg). (more…)
Kazuo Kitagawa, MD PhD
Department of Neurology
Tokyo Women's Medical University
Tokyo, Japan
MedicalResearch.com: What is the background for this study? What are the main findings
Response: Reduction in blood pressure (BP) reduces the rates of recurrent stroke, but the optimum BP target remained unclear.
The results of RESPECT Study together with up-dated meta-analysis showed the benefit of intensive blood pressure lowering (<130/80 mmHg) compared with standard BP lowering (<140/90 mmHg). (more…)
 Kazuo Kitagawa, MD PhD
Department of Neurology
Tokyo Women's Medical University
Tokyo, Japan
MedicalResearch.com: What is the background for this study? What are the main findings
Response: Reduction in blood pressure (BP) reduces the rates of recurrent stroke, but the optimum BP target remained unclear.
The results of RESPECT Study together with up-dated meta-analysis showed the benefit of intensive blood pressure lowering (<130/80 mmHg) compared with standard BP lowering (<140/90 mmHg). (more…)
Kazuo Kitagawa, MD PhD
Department of Neurology
Tokyo Women's Medical University
Tokyo, Japan
MedicalResearch.com: What is the background for this study? What are the main findings
Response: Reduction in blood pressure (BP) reduces the rates of recurrent stroke, but the optimum BP target remained unclear.
The results of RESPECT Study together with up-dated meta-analysis showed the benefit of intensive blood pressure lowering (<130/80 mmHg) compared with standard BP lowering (<140/90 mmHg). (more…)
Author Interviews, Testosterone / 22.07.2019
Testosterone Replacement Therapy Linked to Increased Risk of Heart Attack and Stroke
MedicalResearch.com Interview with:
Christel Renoux, MD, PhD
Assistant Professor, Dept. of Neurology & Neurosurgery
McGill University
Centre For Clinical Epidemiology
Jewish General Hospital - Lady Davis Research Institute
Montreal Canada
MedicalResearch.com: What is the background for this study?
Response: Testosterone replacement therapy is increasingly being prescribed for the treatment of non-specific symptoms among aging men. However, there are concerns regarding the cardiovascular safety of testosterone replacement therapy in aging men and warnings have been issued by health agencies.
(more…)
Author Interviews, Diabetes, Diabetologia, Stroke / 09.06.2019
Midlife Type 2 Diabetes Mellitus Linked to Increased Risk of Ischemic Stroke
MedicalResearch.com Interview with:
Rongrong Yang, PhD candidate
Tianjin Medical University
MedicalResearch.com: What is the background for this study?
Response: Worldwide, cerebrovascular disease (CBD) and type 2 diabetes mellitus (T2DM) are common disorders that have become among the top ten leading causes of death, killing approximately 8 million people in 2016. Both T2DM and CBD are complex genetic and lifestyle-related disorders. Genetic and familial environmental factors (e.g. foetal environment, maternal smoking and childhood socioeconomic status) have been shown to be involved in the development of both conditions. Accumulating evidence from previous studies suggests that T2DM is independently associated with an increased risk of CBD, especially ischemic CBD.
(more…)
Author Interviews, Heart Disease, JAMA, NIH, Stroke / 27.05.2019
Silent Heart Attack Associated with Increased Risk of Embolic Stroke
MedicalResearch.com Interview with:
Lenore J. Launer, PhD.
Chief Neuroepidemiology Section Intramural Research Program
National Institute on Aging
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The prevalence of cerebral infarction on MRI can be as high as 30% in community-based studies. These lesions detected on brain MRI, are often clinically silent, but are associated with impairments in cognitive and physical function and can increase the risk for clinical events. For a large number, the origin of these brain lesions is unknown. There is also a lack of population-based data on unrecognized myocardial infarction, which is associated with an increased for clinical coronary disease and mortality.
Unrecognized MI was detected in 17% of participants using state-of-the-art cardia MRI, a more sensitive measure of the lesions, than the standard ECG. We investigated the contribution to these lesions of recognized and unrecognized myocardial infarction [MI] identified on cardiac MRI.
We found both recognized and unrecognized myocardial infarction increased the risk for cerebral infarction, and that in particular unrecognized MI was associated with cerebral infarction of embolic origins of an unknown source. Given their prevalence, unrecognized MI may be an underestimated contributor to the risk for cerebral infarction in older persons. (more…)
Author Interviews, Brain Injury, Neurological Disorders, Neurology, Stroke / 12.05.2019
Computerized Brain Training BrainHQ Can Reduce Neglect Symptoms of Stroke and Brain Injury
MedicalResearch.com Interview with:
Thomas M Van Vleet PhD
Posit Science
Dr. Tom Van Vleet, presented results on a common symptom of stroke and acquired brain injury (hemi-spatial neglect) at the American Academy of Neurology May 2019
MedicalResearch.com: What makes this study newsworthy?
Response For the first time ever a highly-scalable intervention — computerized brain training (BrainHQ made by Posit Science) —was found to improve symptoms of hemi-spatial neglect, which is a common and often intractable and debilitating problem after stroke or other acquired brain injury.
MedicalResearch.com: What can you tell us about the medical condition (hemi-spatial neglect) investigated in this study?
Response About a third of patients with a brain injury exhibit a complex and debilitating array of neurological deficits known as the “neglect syndrome” (sometimes called, “hemi-spatial neglect” or “neglect”).
The most apparent symptom of neglect is the inability of patients to efficiently process information on the side of space opposite the injury; often completely missing relevant events without awareness. As a result, patients often fail to adopt compensatory strategies or respond to other conventional rehabilitation protocols.
The cost is significant, as patients with neglect experience longer hospital stays and have higher requirements for assistance, including greater skilled nursing home placements relative to patients with similar extent of brain injury without neglect.
To date, there’s been no broadly-applicable and highly-scalable intervention for addressing neglect. An alarming reality given the increasing cost of stroke, which is currently estimated to exceed $34 billion per annum
(more…)
Author Interviews, Clots - Coagulation, NEJM, Neurology / 09.05.2019
Stroke: Thrombolysis Guided by Perfusion Imaging Extended Time Window up to 9 Hours after Onset
MedicalResearch.com Interview with:
Geoffrey A Donnan AO
MBBS, MD, FRCP, FRACP, FAAHMS
Professor of Neurology
University of Melbourne, Melbourne Brain Centre
Royal Melbourne and Austin Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Currently the thrombolysis time window for acute ischemic stroke is restricted to less than 4.5 hours from stroke onset and patients with wake-up stroke are not eligible.
EXTEND is a multi-centre randomised placebo-controlled trial involving patient with acute ischemic stroke who presented between 4.5 to 9 hours of stroke onset or with wake-up-stroke and had penumbral tissue demonstrated on automated perfusion imaging.
Patients were randomised to receive either alteplase or placebo. In total there were 225 patients recruited and the patients who received alteplase had higher rate of excellent functional outcome at 3 months (35.4% vs 29.5% adjusted odd ration 1.44 with 95% confidence interval 1.01 – 2.06 p=0.04). Patients who received alteplase achieved higher rate of early neurological improvement at day 3, reperfusion and recanalization at 24 hours. There was numerically more haemorrhage in the alteplase group but this not negate the functional benefit and there was no difference in the rate of mortality between the two groups. (more…)
AHA Journals, Author Interviews, Clots - Coagulation, Heart Disease, Stroke / 19.04.2019
Stroke: Experimental Antiplatelet Antibody Only Attacks Clots, Without Increasing Bleeding Risk
MedicalResearch.com Interview with:
Martine Jandrot-Perrus MD, PhD.
Emeritus Research Professor
Inserm University Paris Diderot
Acticor Biotech
Hôpital Bichat
France
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Blood platelets are key actors in thrombosis a leading cause of global mortality estimated to account for 1 in 4 death worldwide in 2010.
Thrombosis is associated with cardiovascular diseases (myocardial infarction, stroke, lower limb ischemia, venous thromboembolism), and with numerous pathologies such as cancer, infections or inflammatory diseases. Currently available antiplatelet drugs are the cornerstone of therapy for patients with acute coronary syndromes. However, these drugs all carry an inherent risk of bleeding that restricts their use in sensitive populations and when arterial thrombosis occurs in the cerebral territory. At present the only acute treatment option available for ischemic stroke consists in revascularization by thrombolysis, and/or mechanical thrombectomy. But the number of patients eligible to these treatments is low (» 15% of all patients) and the success rate does not exceed 50%. The responsibility of platelets in the failure for thrombolysis / thrombectomy to restore vascular patency is strongly suspected.
There is thus a clear medical need for new antiplatelet drugs with an improved safety profile. We set out to develop ACT017, a novel, first in class, therapeutic antibody to platelet glycoprotein VI with potent and selective antiplatelet effects. The interest of GPVI resides in the fact that it's a receptor involved in the development of occlusive thrombi but that it is not strictly required for physiological hemostasis.
(more…)
Author Interviews, Brigham & Women's - Harvard, Lipids, Stroke / 16.04.2019
Very Low LDL Cholesterol Associated with Hemorrhagic Stroke in Women
MedicalResearch.com Interview with:
Pamela M. Rist, ScD
Assistant Professor of Medicine, Harvard Medical School
Brigham and Women's Hospital, Division of Preventive Medicine
Boston, MA 02215
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Although hypercholesterolemia is a risk factor for ischemic stroke, some prior studies have observed an inverse association between total and low-density lipoprotein (LDL) cholesterol and risk of hemorrhagic stroke. However, many studies were not able to study this association specifically among women.
Our main result was very low levels of low-density lipoprotein (LDL) cholesterol or low levels of triglycerides were associated with an increased risk of hemorrhagic stroke among women. (more…)
Author Interviews, Diabetes, Geriatrics, Stroke / 06.04.2019
Acetaminophen and Stroke Risk in Diabetic Nursing Home Patients
MedicalResearch.com Interview with:
Philippe Girard, MD,
Gérontopôle de Toulouse, CHU Toulouse
Toulouse, France
MedicalResearch.com: What is the background for this study?
Response: The idea for this study came about in 2016 when a systematic review assessing acetaminophen’s adverse event (AEs) profile came out with results suggesting increased mortality and morbidity (Paracetamol: not as safe as we thought? A systematic literature review of observational studies, PMID: 25732175).
Pr Yves Rolland had collected data from his IQUARE study (Improving the Quality of Care of Long-Stay Nursing Home Residents in France, PMID: 26782872) including all prescriptions from over 6000 nursing home residents and all their medical history over an 18 month follow-up period.
We thought it would be a good idea to assess the safety profile of acetaminophen on this geriatric population. (more…)
Author Interviews, Cognitive Issues, Heart Disease, JAMA, Stroke / 04.03.2019
How Does a Stroke Affect Cognitive Function?
MedicalResearch.com Interview with:
Sarah Parish, MSc, DPhil
Professor of Medical Statistics and Epidemiology
MRC Population Health Research Unit
Nuffield Department of Population Health
University of Oxford
MedicalResearch.com: What is the background for this study?
Response: Acquiring reliable randomized evidence of the effects of cardiovascular interventions on cognitive decline is a priority. In this secondary analysis of 3 randomized intervention trials of cardiovascular event prevention, including 45 029 participants undergoing cognitive testing, we estimated the association of the avoidance of vascular events with differences in cognitive function in order to understand whether reports of non-significant results exclude worthwhile benefit. (more…)
AHA Journals, Artificial Sweeteners, Author Interviews, Stroke / 21.02.2019
Two or More Diet Drinks Per Day Linked to Greater Risk of Stroke
MedicalResearch.com Interview with:
Yasmin Mossavar-Rahmani, Ph.D., RD
Associate Professor
Division of Health Promotion & Nutrition Research
Dept. of Epidemiology & Population Health
Albert Einstein College of Medicine
Bronx, NY 10461
MedicalResearch.com: What is the background for this study?
Response: This is the largest study of the effects of artificially sweetened beverages (ASB) in older women from the Women's Health Initiative Observational Study which started in 1993 and still continues to follow the women. A prior paper indicated excess risk of cardiovascular disease with high consumption of ASBs, but cardiovascular disease was a composite endpoint combining stroke, coronary heart disease, heart failure, revascularization and peripheral arterial disease. Our study focusses on stroke by itself and with different subtypes of stroke. We define high consumption as two or more 12 fl oz. of diet drinks (diet soda or fruit drinks) per day and low consumption as no or less than one drink per week.
(more…)
MedicalResearch.com Interview with:
Sunil A. Sheth, MD
Department of Neurology
McGovern Medical School at UTHealth
Houston, TX 77030
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: There is no country in the world where the absolute number of people living with or died from stroke has declined between 1990 and 2013. In the US, approximately 795,000 people experience a stroke each year with nearly 90% being acute ischemic stroke (AIS), which remains the leading cause of adult disability in the US.
In 2015 landmark clinical trials demonstrated that endovascular stroke treatments (EST) for patients with large vessel occlusion (LVO) leads to dramatic improvements in patient outcomes. However, in the wake of these results, stroke systems of care around the globe are now faced with the daunting task of ensuring that patients with AIS have access to appropriate screening and therapy.
The evidence of benefit for endovascular stroke that emerged from these trials was derived from treatments rendered almost exclusively at high volume stroke centers, with specialized neuro-imaging, neuro-intensive care, neuro-rehabilitation and neuro-nursing. However, since the publication and adoption of these findings into guidelines, it has become well-established that the likelihood of good neurologic outcome for these patients remains dependent on minimizing delays in treatment. Even 15-minute delays in endovascular reperfusion have been associated with quantifiable decrements in clinical outcomes. As such, there has been an increase in demand for the procedure as well as calls for the dissemination of the treatment away from tertiary-care referral centers into the community, to avoid the costly delays associated with inter-hospital transfer (IHT). On the other hand, transferring endovascular stroke patients to higher volume centers has also been associated with reduced mortality. In the absence of clear data on the relative efficacy of EST in lower volume centers, this lack of clarity on the optimal distribution of endovascular stroke resources had led to considerable confusion, with stroke center certifying agencies such as The Joint Commission initially requiring physician and hospital minimal EST volume requirements for certification, and then very recently revoking and then reinstating that criterion.
Given the need to structure stroke systems of care in the modern endovascular stroke era, as well as the poorly characterized effect on EST outcomes away from tertiary-care referral centers, understanding the trends in treatment patterns as well as outcomes in relation to treatment volumes and IHT is of vital importance. The study described here provides for the first time large-scale data on the utilization of the procedure as well as the finding that its outcomes are directly tied to annual volumes.
(more…)
Author Interviews, Genetic Research, JAMA, Race/Ethnic Diversity, Stroke / 11.02.2019
Link Between Apolipoprotein E and Brain Hemorrhage Varies by Ethnicity
MedicalResearch.com Interview with:
Sandro Marini, MD
Research Fellow
Jonathan Rosand Laboratory
Massachusetts General Hospital
Boston, MA 02114
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The epsilon(ε) 4 allele of the Apolipoprotein E (APOE) gene increases risk for Alzheimer’s disease (AD) and intracerebral hemorrhage (ICH).
In both diseases, it is believed to increase risk through the deposition of beta-amyloid within the brain and blood vessels, respectively. The effect of APOE ε4 on both AD and ICH risk changes across populations, for unclear reasons.
In our study, we confirmed the role of APOE ε4 for ICH risk in whites and found that the risk-increasing effect of the 4 allele is demonstrable in Hispanics only when balancing out the effect of hypertension.
(more…)
Author Interviews, Health Care Systems, JAMA, Stroke, University Texas / 11.02.2019
Stroke: Outcomes of Patients Transferred for Thrombectomy
MedicalResearch.com Interview with:
Amrou Sarraj, MD, Associate Professor
Department of Neurology
McGovern Medical School
The University of Texas Health Science Center at Houston.
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Secondary analyses of trials showing efficacy and safety of thrombectomy within 6-8 hours of stroke onset showed that patients who were transferred to centers performing thrombectomy from another hospital had worse outcomes than patients who presented directly to the thrombectomy centers. We wanted to assess if the thrombectomy outcomes differ between transferred patients and patients directly coming to the thrombectomy centers when patients are selected with advanced perfusion imaging.
We found that thrombectomy outcome rates were similar between patients who presented directly vs transferred from another hospital, including functional independence and safety outcomes.
(more…)
Author Interviews, Diabetes, JAMA, Metabolic Syndrome, Stroke / 10.02.2019
Pioglitazone (Actos) Reduced Risk of Secondary Stroke and New Onset of Diabetes
MedicalResearch.com Interview with:
David Spence M.D., FRCPC, FAHA
Professor of Neurology and Clinical Pharmacology
Director, Stroke Prevention & Atherosclerosis Research Centre,
Robarts Research Institute, Western University
London, ON Canada
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The motivation for the study was the chair of the committee that advises the Ontario Drug Benefit which medications to pay for said the IRIS results were not relevant to clinical practice. This because the Insulin Resistance Intervention after Stroke (IRIS) trial reported effects of pioglitazone in patients with stroke or TIA and insulin resistance assessed by the Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) score for insulin resistance.1 ( However, few clinicians measure a HOMA-iR score, so the clinical impact of that trial was limited.
In this study we analyzed the effect of pioglitazone in stroke/TIA patients with prediabetes, which is commonly assessed by clinicians. Prediabetes was defined by the American Diabetes Association: a glycosylated hemoglobin (A1C) of 5.7% to <6.5% (we did not do glucose tolerance tests). We analyzed primarily the results for patients with 80% adherence, but also did an intention-to-treat (ITT) analysis. The reason for focusing on patients with good adherence was that pioglitazone cannot be taken by about 10-20% of patients, because of fluid retention and weight gain (mainly due to fluid retention). (The reasoning was that third party payers would not need to pay for the medication in patients who do not take it.)
In stroke/TIA patients with good adherence, the benefits of pioglitazone were greater than in the original IRIS trial. We found a 40% reduction of stroke/MI, a 33% reduction of stroke, and an 80% reduction of new-onset diabetes, over 5 years. Pioglitazone also improved blood pressure, triglycerides and HDL-cholesterol. As expected, pioglitazone was somewhat less beneficial in the ITT analysis.
Fluid retention can usually be managed by reducing the dose of pioglitazone; even small doses still have a beneficial effect . Also, amiloride has been shown to reduce fluid retention with pioglitazone.
- Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, Guarino PD, Lovejoy AM, Peduzzi PN, Conwit R, Brass LM, Schwartz GG, Adams HP, Jr., Berger L, Carolei A, Clark W, Coull B, Ford GA, Kleindorfer D, O'Leary JR, Parsons MW, Ringleb P, Sen S, Spence JD, Tanne D, Wang D, Winder TR and Investigators IT. Pioglitazone after Ischemic Stroke or Transient Ischemic Attack. N Engl J Med. 2016;374:1321-31.
AHA Journals, Author Interviews, Diabetes, Stroke / 08.02.2019
Stroke: Intensive Blood Sugar Control Did Not Improve Outcomes
MedicalResearch.com Interview with:
Karen C. Johnston MD
Professor and Chair, Neurology
School of Medicine
University of Virginia
MedicalResearch.com: What is the background for this study?
Response: We know that acute ischemic stroke patient with hyperglycemia at presentation have worse outcomes. We also know if we lower the glucose too low that this is bad for ischemic brain also. T
he SHINE trial addressed a world wide debate about whether intensive treatment of hyperglycemia is beneficial. We assessed the efficacy and safety of an intensive glucose control protocol with a target glucose of 80-130 mg/dL compared to a more standard protocol with a target of less than 180 mg/dL.
(more…)
Author Interviews, Pain Research, Stroke / 04.02.2019
Dive Deep Into Migraine’s Link to Increased Stroke Incidence
MedicalResearch.com Interview with
Michelle Androulakis, MD, MS, FAHS
Chief of Neurology
WJB Dorn VA Medical Center and
Faculty at University of South Carolina.
Columbia, SC
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Even though Migraine with aura was associated with an increased risk of ischemic stroke in the Atherosclerosis Risk in Communities study (ARIC), our post-hoc showed unexpected results that onset of such migraines before age 50 years is not associated with such risk. Instead, later onset of migraine with aura after age of 50 was linked with a higher risk of ischemic stroke.
Total of 447 migraineurs with aura (MA) and 1128 migraineurs without aura (MO) among 11,592 participants were included in the analysis. There was a two-fold increased risk of ischemic stroke when the age of migraineurs with aura onset was 50 years or older as compared with no headache participants, MO was not associated with increased stroke risk regardless of age of onset. (more…)
Author Interviews, Global Health, Stroke / 26.12.2018
Stroke Prevention Should Begin in Young Adults
MedicalResearch.com Interview with:
Gregory A. Roth MD MPH
Assistant Professor, Medicine - Cardiology
Adjunct Assistant Professor, Global Health
Adjunct Assistant Professor, Health Metrics Sciences
School of Public Health
University of Washington
Seattle, WA
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: We found that globally, one in four people over age 25 is at risk for stroke during their lifetime. But we also found large geographic variation, including a nearly five-fold difference in lifetime stroke risk worldwide, with the highest risk in East Asia (38.8%), Central Europe (31.7%), and Eastern Europe (31.6%), and the lowest risk in eastern sub-Saharan Africa (11.8%). Chinese men and Latvian women had the world’s highest estimated lifetime stroke risk in 2016. The lifetime stroke risk on average for 25-year-olds in 2016 ranges from 8% to 39%, depending on the country in which they live.
This is the first time a study has produced estimates of lifetime stroke risk starting at age 25, whereas previous studies begin at age 45. These findings suggest that adults need to think about their long-term health risks, including stroke, at a much younger age. Additionally, one’s risk of stroke over the course of your lifetime depends on where you live. Given the burden of stroke among adults is dependent on modifiable risk factors and the characteristics of health systems, our findings may be useful for long-term planning, especially in terms of prevention and public education. (more…)