Author Interviews, Immunotherapy, Kidney Disease, NEJM / 15.01.2024
NEJM: Sibeprenlimab Stabilized Kidney Function Decline in Most Common Glomerular Disease
MedicalResearch.com Interview with:
 Mohit Mathur MD, FASN, FNKF, FRCP (Glasgow)
Clinical fellow in Nephrology at UofT
DM (Nephrology), MRCP.UK (SCE in Nephrology).
Director, Clinical Development
Visterra
Waltham, MA 02451
MedicalResearch.com: What is the background for this study? Would you briefly describe the condition of IgA Nephropathy?
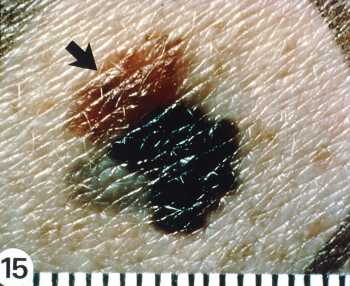
Response: IgA Nephropathy is the commonest primary glomerular disease in the world. It is an autoimmune kidney disease that typically presents with urinary abnormalities, elevated blood pressure and reduced kidney function. Until recently IgAN was considered to be a benign disease, but recent studies have indicated that a majority of patients will progress to End stage kidney disease in their lifetime.
Steroids have been the mainstay of treatment in IgAN, but they come at a very high burden of side effects. Thus, there is an urgent requirement to develop novel and safe treatment options for patients with IgAN. APRIL is considered to be a key cytokine implicated in the pathogenesis of IgAN, hence we decided to target APRIL as a therapeutic modality in IgAN.
(more…)
Mohit Mathur MD, FASN, FNKF, FRCP (Glasgow)
Clinical fellow in Nephrology at UofT
DM (Nephrology), MRCP.UK (SCE in Nephrology).
Director, Clinical Development
Visterra
Waltham, MA 02451
MedicalResearch.com: What is the background for this study? Would you briefly describe the condition of IgA Nephropathy?
Response: IgA Nephropathy is the commonest primary glomerular disease in the world. It is an autoimmune kidney disease that typically presents with urinary abnormalities, elevated blood pressure and reduced kidney function. Until recently IgAN was considered to be a benign disease, but recent studies have indicated that a majority of patients will progress to End stage kidney disease in their lifetime.
Steroids have been the mainstay of treatment in IgAN, but they come at a very high burden of side effects. Thus, there is an urgent requirement to develop novel and safe treatment options for patients with IgAN. APRIL is considered to be a key cytokine implicated in the pathogenesis of IgAN, hence we decided to target APRIL as a therapeutic modality in IgAN.
(more…)