MedicalResearch.com Interview with:
Dr. Ingunn Olea Lund, PhD
The Norwegian Institute of Public Health
Oslo, Norway
MedicalResearch.com: What is the background for this study?
Response: There are significant amounts of research on children of parents with alcohol use disorders – where the children are shown to be at risk of several adverse outcomes, including mental disorders, substance use disorders, suicide, impaired school performance, and employment problems. There is very little previous research on how other, more normal levels of parental drinking may influence child outcomes, such as mental health. This is a grave oversight, as there are vastly more parents with normal drinking patterns than there are parents who suffer from an alcohol use disorder. This means that there are potentially a lot more cases of adverse effect for children, and the number of children at risk may be higher than previously assumed.
In addition to parents' alcohol use, several other risk factors in the family that may affect child mental health outcomes, such as parents' mental health and socio-economic status. Researchers have tended to look at these risk factors separately, but as these risks tend to co-occur, it may be more informative to consider them together.
To our knowledge, this is the first study that examines possible harm from normal levels of parental drinking, alone or in combination with other parental risk factors, on children’s anxiety and depression.
The sample consists of more than 8700 triads: children and both their parents. We combined information from three health registries with survey data where both adolescents and their parents provided information about health and social conditions. The health registers include information about the children 's actual contact with the health care system; we used information about whether children received diagnoses and/or treatment for anxiety and/or depression.
(more…)







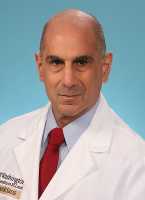













 Yingxi (Cimo) Chen, MD, MPH, PhD
Postdoctoral Fellow
Radiation Epidemiology Branch, DCEG, NCI, NIH
Rockville MD 20850
MedicalResearch.com: What is the background for this study?
Response: Death rates from drug overdose have more than doubled in the US in the 21st century. Similar increases in drug overdose deaths have been reported in other high-income countries but few studies have compared rates across countries.
Yingxi (Cimo) Chen, MD, MPH, PhD
Postdoctoral Fellow
Radiation Epidemiology Branch, DCEG, NCI, NIH
Rockville MD 20850
MedicalResearch.com: What is the background for this study?
Response: Death rates from drug overdose have more than doubled in the US in the 21st century. Similar increases in drug overdose deaths have been reported in other high-income countries but few studies have compared rates across countries. 




