Author Interviews, Cost of Health Care, CT Scanning, Heart Disease, JACC, Statins / 14.01.2021
Calcium Artery Score Screening: Cost Effectiveness in Patients with Family History of Early Heart Disease
MedicalResearch.com Interview with:
Prasanna Venkataraman MBBS
Thomas H. Marwick MBBS, PhD
Baker Heart and Diabetes Research Institute
Monash University, Melbourne
Melbourne, Australia
MedicalResearch.com: What is the background for this study?
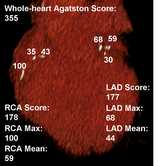
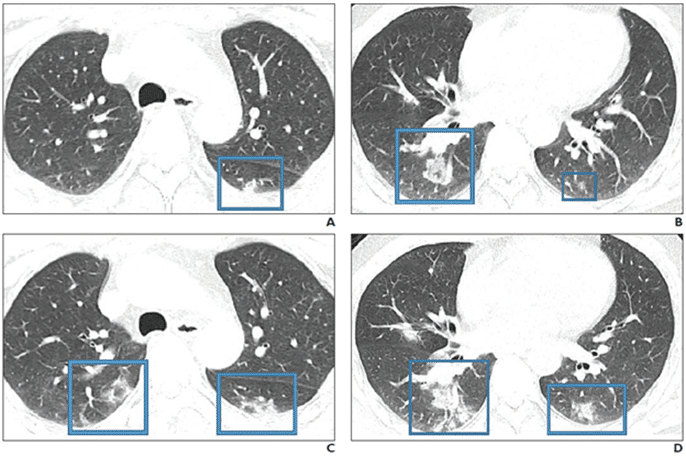
- Coronary artery calcium score (CAC) quantifies coronary calcium as determined by computed tomography and is a good surrogate marker for overall coronary plaque burden. It can help to reclassify patients at intermediate risk – many of whom are actually at low risk and can be reassured. Conversely, the finding of coronary calcium can also motivate patients (and their clinicians) to more aggressively control their cardiovascular risk factors. This is particularly problematic in those with a family history of premature coronary artery disease, where standard risk prediction tools are less accurate. However, CT CAC does not routinely attract third party payer support limiting its access and utilisation.
- We screened 1084 participants who have a family history of premature coronary disease and a 10-year Pooled cohort Equation (PCE) cardiovascular risk >2% with CAC. We then assessed the cost-effectiveness of commencing statins in those with any coronary calcium compared to a strategy of no CAC testing and commencing statins if their PCE risk was ≥7.5% consistent with current guidelines.