Clinical Score Predicts Recovery From Dialysis Dependent Acute Kidney Injury
NEJM: UTSW Study Evaluates Whether Practice Facilitators Reduce Hospitalizations in CKD Patients
AHA23: Unexpected Link Between Sleep Apnea and Cardiovascular Events in Kidney Disease Patients
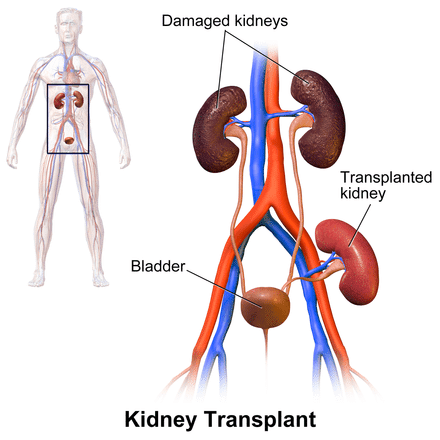
Kidney Transplant and Living Kidney Donation: Multicomponent Program to Improve Patient Access
- Patients with advanced chronic kidney disease (CKD) have the best chance for a longer and healthier life if they receive a kidney transplant.
- However, due to many barriers, many eligible patients today will never receive a kidney transplant.
- Advanced CKD care is provided by 26 chronic kidney disease (CKD) programs managed by a government funded provincial renal agency (the Ontario Renal Network)
- Together these 26 programs treat ~ 24,000 patients each year
- This care is provided by over 3400 nurses and 230 nephrologists
- To patients approaching the need for dialysis and those receiving dialysis
- Approximately half are transplant eligible
- ~ 600 kidney transplants done in Ontario each year across 6 transplant centres
- with approximately.30% of kidneys coming from living donors
Hemodialysis: Canadian Study Describes Improved Membrane to Reduce Complications
Associate Professor, Chemical and Biomedical Engineering
Department of Chemical and Biological Engineering
Division of Biomedical Engineering
University of Saskatchewan MedicalResearch.com: What is the background for this study? Response: The background of this study lies in the pursuit of improving the compatibility of dialysis membranes used in hospitals. My team sought to enhance the performance of these membranes by incorporating heparin, a widely recognized anticoagulant. Existing heparin-grafted membranes carried a negative charge, resulting in adverse blood-membrane interactions and complications for dialysis patients. The study aimed to overcome these issues and create a neutralized membrane surface that maintains the benefits of heparin while minimizing undesirable interactions. (more…)
UCSF Study Finds Acute Kidney Injury Does Not Worsen Course of CKD
Study Finds Reduced Kidney Disease Progression with DOACs vs Vitamin K Antagonists
Increased Adrenal Hormone Aldosterone Linked to Greater Risk of Chronic Kidney Disease
Lilly’s Tirzepatide Slowed Kidney Function Decline in High Risk Diabetics with Heart Disease
Chronic Kidney Disease: Study Evaluates What Happens to Patients Who Forgo Dialysis
Facilities that Care For Poor Kidney Failure Patients Can Be Financially Penalized
Low Dose Aspirin May Be Beneficial in Chronic Kidney Disease Patients
Investigators Find Removing Race Coefficient from CKD-EPI Equation Would Introduce Bias Rather Than Improve Accuracy
Chronic Kidney Disease: More Patients Would Benefit from Lower Blood Pressure Targets


Re-evaluation of Race Multiplier in Estimating Kidney Disease
The original CKD-EPI and MDRD studies showed an association between African-American race with higher measured GFR at the same blood creatinine concentration. However, there have been concerns raised about the application of the race multiplier to all African-American patients. First, there is no clear biological explanation for the association, the identification of Black race was unclear in some of the cohorts used in these studies, and there is vast genetic and ancestral heterogeneity among those who self-identify as black. The use of the race multiplier also ignores the fact that race is a social, not biological construct.
We found that with the removal of the race multiplier, up to one in every three African-American patients would be reclassified as having a more severe stage of CKD, with one-quarter of African-American patients going from stage 3 to stage 4. We also found that with the removal of the race multiplier, 64 patients would have had an eGFR <20, the threshold for referral for kidney transplant, and none of these patients were referred, evaluated or waitlisted for transplant. This is in contrast, to those African-American patients with an eGFR <20 with the race multiplier applied, who had a higher odds of being referred, evaluated or waitlisted for transplant compared to other racial groups (Odds ratio of 2.28, compared to White cohort).
(more…)Study Finds Novel Difelikefalin (Korsuva) Stops the Itch of Chronic Kidney Disease
Fewer Kidney Failure Patients Rely on Medicare for Dialysis
Researchers Regenerate Functioning Kidney Cells from Patients With Chronic Renal Disease
Disparities Persist Between Kidney Transplantation and Dialysis Facility Ownership
French More Likely to Transplant Kidneys from Older, Sicker Patients
Oral Anticoagulant in Chronic Kidney Disease: Benefits and Harms
Many Dialysis Patients Do Not Think of Themselves As Having a Life Limiting Condition
Angion Receives Support to Develop Drug Candidate for a Scarring Form of Kidney Disease, FSGS
Chronic Kidney Disease: Exome Sequencing Can Help Resolve Some Diagnostic Challenges
Chronic Kidney Disease Rate Rising Faster Than Other Noncommunicable Diseases
Medicaid Expansion Linked To Lower Death Rates for Kidney Failure Patients


New Drug Class Offers Hope for Calcified Blood Vessels
Is there an Association between Cannabis and Acute Kidney Injury in CKD Patients?


Biomarkers Suggest Intensive Blood Pressure Treatment Does Not Cause True Kidney Damage in CKD Patients
- Our study represents major advancements in our understanding of whether kidney tissue damage accompanies the diagnosis of chronic kidney disease during hypertension therapy.
- The Systolic Blood Pressure Intervention Trial (SPRINT) was a landmark clinical trial that demonstrated that more intensive systolic blood pressure management (target <120 mmHg) reduced rates of major cardiovascular events and mortality compared with standard therapy (<140 mmHg). A recent announcement indicated that the lower systolic blood pressure target also slowed the rate of cognitive decline and dementia incidence.
- The major concern with intensive blood pressure lowering in SPRINT is the 3-fold incidence of chronic kidney disease, as defined using the clinical standard of serum creatinine levels. This detrimental impact on the kidney was surprising because hypertension is a predominant risk factor for kidney disease, and hypertension therapy should reduce CKD risk.
- Given the lower blood pressure targets in the recently-updated national hypertension guidelines, there has been substantial concern that guideline implementation of blood pressure targets could cause an epidemic of CKD and the attendant suffering from its downstream consequences of cardiovascular disease, heart failure, and kidney failure.
- In our study, we compared SPRINT participants who developed CKD with matched controls, using a panel of validated urinary biomarkers of kidney damage. These urine tests can measure actual kidney damage, rather than relying on the creatinine which is an indirect reflection of the kidney’s filtering function.
- In the group undergoing intensive blood pressure lowering in SPRINT, we found that the new cases of CKD had an overall lowering of the kidney damage biomarkers compared with the controls, contrary to what would have been expected if they were developing “real” CKD.
- In contrast, the new CKD cases that developed in the standard treatment group did have overall elevations in the urinary biomarkers of kidney damage; 5 of the 9 biomarkers significantly increased relative to the CKD cases in the intensive treatment group.
- 1
- 2