Obstructive Sleep Apnea Common in Patients with Resistant Hypertension
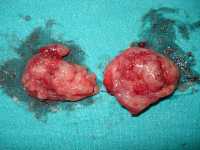
Is There a Risk of Bleeding With Ibuprofen After Tonsillectomy ?
Undiagnosed Sleep Apnea Linked to Resistant Hypertension in African Americans
Tonsillectomy Often Done When Not Indicated (and vice versa!)
Obstructive Sleep Apnea: Short Apneas Linked To Increased Mortality
 Matthew P Butler, PhD
Assistant Professor, Oregon Institute of Occupational Health Sciences
Assistant Professor, Department of Behavioral Neuroscience
Oregon Health & Science University
Portland, OR 97239
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Obstructive sleep apnea (OSA) is associated with heart disease and mortality, but how OSA does this is not well understood. We are therefore looking for sub-phenotypes within OSA that will help us predict who is at greatest risk.
Current diagnosis of OSA is made on the basis of the apnea-hypopnea index (AHI – the number of respiratory events per hour of sleep). But the AHI is not a very good predictor of future mortality.
We tested the hypothesis that the duration of events (how long the breathing interruptions are) would predict risk. We found that those with the shortest breathing interruptions had the highest risk of dying, after accounting for other conditions like age, gender, race, and smoking status. (more…)
Matthew P Butler, PhD
Assistant Professor, Oregon Institute of Occupational Health Sciences
Assistant Professor, Department of Behavioral Neuroscience
Oregon Health & Science University
Portland, OR 97239
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Obstructive sleep apnea (OSA) is associated with heart disease and mortality, but how OSA does this is not well understood. We are therefore looking for sub-phenotypes within OSA that will help us predict who is at greatest risk.
Current diagnosis of OSA is made on the basis of the apnea-hypopnea index (AHI – the number of respiratory events per hour of sleep). But the AHI is not a very good predictor of future mortality.
We tested the hypothesis that the duration of events (how long the breathing interruptions are) would predict risk. We found that those with the shortest breathing interruptions had the highest risk of dying, after accounting for other conditions like age, gender, race, and smoking status. (more…)People With Sleep Apnea At Increased Risk of Gout
Structural Brain Changes in Sleep Apnea Linked to Cognitive Decline
 Nathan E. Cross PhD, first author
School of Psychology.
Sharon L. Naismith, PhD, senior author
Leonard P Ullman Chair in Psychology
Brain and Mind Centre
Neurosleep, NHMRC Centre of Research Excellence
The University of Sydney, Australia
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Between 30 to 50% of the risk for dementia is due to modifiable risk factors such depression, hypertension, physical inactivity, obesity, diabetes and smoking.
In recent years, multiple longitudinal cohort studies have observed a link between sleep apnoea and a greater risk (1.85 to 2.6 times more likely) of developing cognitive decline and dementia. Furthermore, one study in over 8000 people also indicated that the presence of obstructive sleep apnoea (OSA) in older adults was associated with an earlier age of cognitive decline, and that treatment of OSA may delay the onset of cognitive impairment.
This study reveals important insights into how sleep disorders such as OSA may impact the brain in older adults, as it is associated with widespread structural alterations in diverse brain regions. We found that reduced blood oxygen levels during sleep are related to reduced thickness of the brain's cortex in both the left and right temporal areas - regions that are important in memory and are early sites of injury in Alzheimer's disease. Indeed, reduced thickness in these regions was associated with poorer ability to learn new information, thereby being the first to link this structural change to memory decline. (more…)
Nathan E. Cross PhD, first author
School of Psychology.
Sharon L. Naismith, PhD, senior author
Leonard P Ullman Chair in Psychology
Brain and Mind Centre
Neurosleep, NHMRC Centre of Research Excellence
The University of Sydney, Australia
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Between 30 to 50% of the risk for dementia is due to modifiable risk factors such depression, hypertension, physical inactivity, obesity, diabetes and smoking.
In recent years, multiple longitudinal cohort studies have observed a link between sleep apnoea and a greater risk (1.85 to 2.6 times more likely) of developing cognitive decline and dementia. Furthermore, one study in over 8000 people also indicated that the presence of obstructive sleep apnoea (OSA) in older adults was associated with an earlier age of cognitive decline, and that treatment of OSA may delay the onset of cognitive impairment.
This study reveals important insights into how sleep disorders such as OSA may impact the brain in older adults, as it is associated with widespread structural alterations in diverse brain regions. We found that reduced blood oxygen levels during sleep are related to reduced thickness of the brain's cortex in both the left and right temporal areas - regions that are important in memory and are early sites of injury in Alzheimer's disease. Indeed, reduced thickness in these regions was associated with poorer ability to learn new information, thereby being the first to link this structural change to memory decline. (more…)CPAP Improved Sexual Quality of Life for Women
MedicalResearch.com Interview with: [caption id="attachment_38315" align="alignleft" width="200"] One CPAP modelImage by Bryan Alexander[/caption] Sebastian M. Jara, MD Resident Physician & Research Fellow Department of...
Sleep Apnea Increases Amyloid Load In Brain, A Hallmark of Alzheimer’s Disease
Women With Severe Hot Flashes At Higher Risk of Obstructive Sleep Apnea
Sleep-Disordered Breathing Associated With Increased Risk of Cognitive Impairment
Adaptive Servo-Ventilation Therapy Has Variable Effects in Heart Failure Patients
Drug-Induced Sleep Endoscopy With Cardiorespiratory Monitoring For OSA
Vitamin D Level Likely Has No Impact on Sleep Apnea
Both CPAP and Mandibular Advancement Devices Improve Blood Pressure in Sleep Apnea
[caption id="attachment_19645" align="alignleft" width="140"] Dr. Kohler[/caption] MedicalResearch.com Interview with: Prof. Malcolm Kohler, MD Chair Respiratory Medicine Clinical Director Department of Pulmonology University Hospital of Zurich Zurich...
Surgical Treatment An Option For Patients With Recalcitrant Sleep Apnea
Cost-Effective Clinical Pathway Determined Hospitalized Patients’ Risk of Sleep Apnea
 MedicalResearch.com Interview with:
Sunil Sharma, M.D
Associate professor of pulmonary medicine
Sidney Kimmel Medical College at Thomas Jefferson University
Medical Research: What is the background for this study? What are the main findings?
Dr. Sharma: Obstructive sleep apnea (OSA) is a highly prevalent disorder with significant cardiovascular implications. In this condition the patient may repeatedly quit breathing during sleep, sometimes hundreds of times, leading to loss of oxygen and frequent arousals throughout the night. OSA has been associated with high blood pressure, congestive heart failure, coronary artery disease, arrhythmias and stroke, among other conditions. While overall awareness is improving, the condition is under-recognized in hospitalized patients. Due to multiple co-morbid conditions these patients may be at higher risk for complications. Recent studies have also shown that early recognition of OSA in hospitalized patients may reduce readmission rates. In our study, we used a simple and cost-effective clinical pathway to determine high-risk patients. Of the 149 patient's determined to be high risk by our protocol, 128 (87%) were confirmed with the diagnosis by a polysomnography (gold standard test). Furthermore, data derived from a simple and cost-effective oxygen measuring device (pulse-oximeter) was found to co-relate well with the polysomnography. (more…)
MedicalResearch.com Interview with:
Sunil Sharma, M.D
Associate professor of pulmonary medicine
Sidney Kimmel Medical College at Thomas Jefferson University
Medical Research: What is the background for this study? What are the main findings?
Dr. Sharma: Obstructive sleep apnea (OSA) is a highly prevalent disorder with significant cardiovascular implications. In this condition the patient may repeatedly quit breathing during sleep, sometimes hundreds of times, leading to loss of oxygen and frequent arousals throughout the night. OSA has been associated with high blood pressure, congestive heart failure, coronary artery disease, arrhythmias and stroke, among other conditions. While overall awareness is improving, the condition is under-recognized in hospitalized patients. Due to multiple co-morbid conditions these patients may be at higher risk for complications. Recent studies have also shown that early recognition of OSA in hospitalized patients may reduce readmission rates. In our study, we used a simple and cost-effective clinical pathway to determine high-risk patients. Of the 149 patient's determined to be high risk by our protocol, 128 (87%) were confirmed with the diagnosis by a polysomnography (gold standard test). Furthermore, data derived from a simple and cost-effective oxygen measuring device (pulse-oximeter) was found to co-relate well with the polysomnography. (more…)Custom Oral Appliance Reduced Sleep Apnea and Restless Legs
 MedicalResearch.com Interview with:
Marie Marklund, DDS senior lecturer
Department of Odontology, Faculty of Medicine
Umeå University
Sweden
MedicalResearch: What is the background for this study? What are the main findings?
Response: Snoring and obstructive sleep apnea are common in the population and these disorders continuously increase because of the ongoing obesity epidemic in many countries. Today, 34% of men and 17% of women in the US suffer from obstructive sleep apnea of all severities. Symptoms include daytime sleepiness, poor sleep quality, headache, insomnia and restless legs. In the longer term, a more severe sleep apnea is associated with serious consequences, such as hypertension, stroke, cancer, traffic accidents and early death.
Continuous positive airway pressure is a highly effective treatment for sleep apnea patients. Adherence problems, for instance from nasal stuffiness and claustrophobia reduces its effectiveness. An oral appliance holds the lower jaw forwards during sleep in order to reduce snoring and sleep apneas. This therapy has primarily been suggested for snorers and patients with mild and moderate sleep apnea. No previous placebo-controlled study has, however, evaluated this specific group of patients. Results from more severe sleep apnea patients have shown a good effect on sleep apneas. The effect of oral appliances on daytime symptoms is unclear. Symptomatic improvement is an important outcome for milder sleep apnea patients.
The primary aims of the present study were to study the effects on daytime sleepiness and quality of life of a custom-made, adjustable oral appliance in patients with daytime sleepiness and snoring or mild to moderate sleep apnea, i.e. the primary target group for this type of therapy. Secondary aims included the effects on sleep apnea, snoring and various other symptoms of sleep disordered breathing such as headaches and restless legs. We found that oral appliance therapy was effective in reducing sleep apneas, snoring and symptoms of restless legs. The apnea-hypopnea index was normal (<5) in 49% of patients using the active appliance and in 11% using placebo, with a numbers needed to treat of three. Daytime sleepiness and quality of life did not differ during active treatment and the placebo intervention. The patients experienced reduced headaches with active treatment, but the results did not differ from placebo. It was concluded, that a custom-made, adjustable oral appliance reduces obstructive sleep apneas, snoring and possibly restless legs. The efficacy on daytime sleepiness and quality of life was weak and did not differ from placebo in this group of patients. (more…)
MedicalResearch.com Interview with:
Marie Marklund, DDS senior lecturer
Department of Odontology, Faculty of Medicine
Umeå University
Sweden
MedicalResearch: What is the background for this study? What are the main findings?
Response: Snoring and obstructive sleep apnea are common in the population and these disorders continuously increase because of the ongoing obesity epidemic in many countries. Today, 34% of men and 17% of women in the US suffer from obstructive sleep apnea of all severities. Symptoms include daytime sleepiness, poor sleep quality, headache, insomnia and restless legs. In the longer term, a more severe sleep apnea is associated with serious consequences, such as hypertension, stroke, cancer, traffic accidents and early death.
Continuous positive airway pressure is a highly effective treatment for sleep apnea patients. Adherence problems, for instance from nasal stuffiness and claustrophobia reduces its effectiveness. An oral appliance holds the lower jaw forwards during sleep in order to reduce snoring and sleep apneas. This therapy has primarily been suggested for snorers and patients with mild and moderate sleep apnea. No previous placebo-controlled study has, however, evaluated this specific group of patients. Results from more severe sleep apnea patients have shown a good effect on sleep apneas. The effect of oral appliances on daytime symptoms is unclear. Symptomatic improvement is an important outcome for milder sleep apnea patients.
The primary aims of the present study were to study the effects on daytime sleepiness and quality of life of a custom-made, adjustable oral appliance in patients with daytime sleepiness and snoring or mild to moderate sleep apnea, i.e. the primary target group for this type of therapy. Secondary aims included the effects on sleep apnea, snoring and various other symptoms of sleep disordered breathing such as headaches and restless legs. We found that oral appliance therapy was effective in reducing sleep apneas, snoring and symptoms of restless legs. The apnea-hypopnea index was normal (<5) in 49% of patients using the active appliance and in 11% using placebo, with a numbers needed to treat of three. Daytime sleepiness and quality of life did not differ during active treatment and the placebo intervention. The patients experienced reduced headaches with active treatment, but the results did not differ from placebo. It was concluded, that a custom-made, adjustable oral appliance reduces obstructive sleep apneas, snoring and possibly restless legs. The efficacy on daytime sleepiness and quality of life was weak and did not differ from placebo in this group of patients. (more…)CPAP For Sleep Apnea May Decrease Atrial Fibrillation Recurrence
 MedicalResearch.com Interview with:
Dr. Larry Chinitz MD
Professor of Medicine and Director, Cardiac Electrophysiology
NYU Langone Medical Center
MedicalResearch: What is the background for this study? What are the main findings?
Dr. Chinitz: The treatment algorithms proposed currently for maintenance of sinus rhythm in patients with atrial fibrillation focus on use of anti-arrhythmic drugs and catheter ablation. Data available to evaluate the effect of modification of known adverse clinical factors on atrial fibrillation recurrence is scant.
Obstructive sleep apnea in a known factor associated with both new onset atrial fibrillation as well as its recurrence after catheter ablation. Through a meta-analysis of available data we found that use of continuous positive airway pressure in patients with sleep apnea was associated with a 42% relative risk reduction in recurrence of atrial fibrillation. This effect was similar across patient groups irrespective of whether they were medically managed or with catheter ablation.
(more…)
MedicalResearch.com Interview with:
Dr. Larry Chinitz MD
Professor of Medicine and Director, Cardiac Electrophysiology
NYU Langone Medical Center
MedicalResearch: What is the background for this study? What are the main findings?
Dr. Chinitz: The treatment algorithms proposed currently for maintenance of sinus rhythm in patients with atrial fibrillation focus on use of anti-arrhythmic drugs and catheter ablation. Data available to evaluate the effect of modification of known adverse clinical factors on atrial fibrillation recurrence is scant.
Obstructive sleep apnea in a known factor associated with both new onset atrial fibrillation as well as its recurrence after catheter ablation. Through a meta-analysis of available data we found that use of continuous positive airway pressure in patients with sleep apnea was associated with a 42% relative risk reduction in recurrence of atrial fibrillation. This effect was similar across patient groups irrespective of whether they were medically managed or with catheter ablation.
(more…)Sleep Apnea Increases Stroke Risk in Atrial Fibrillation Patients
 MedicalResearch.com Interview with:
Dmitry Yaranov, MD
Danbury Hospital
Western Connecticut Health Network
Medical Research: What is the background for this study? What are the main findings?
Dr. Yaranov: Obstructive sleep apnea (OSA) is an independent risk factor for ischemic stroke (CVA) that is not included in the usual cardioembolic risk assessments for patients with atrial fibrillation. The aim of this study was to investigate the impact of OSA on CVA rate in patients with atrial fibrillation. We found that Obstructive sleep apnea in patients with atrial fibrillation is an independent predictor of CVA and this association may have important clinical implications in CVA risk stratification. (more…)
MedicalResearch.com Interview with:
Dmitry Yaranov, MD
Danbury Hospital
Western Connecticut Health Network
Medical Research: What is the background for this study? What are the main findings?
Dr. Yaranov: Obstructive sleep apnea (OSA) is an independent risk factor for ischemic stroke (CVA) that is not included in the usual cardioembolic risk assessments for patients with atrial fibrillation. The aim of this study was to investigate the impact of OSA on CVA rate in patients with atrial fibrillation. We found that Obstructive sleep apnea in patients with atrial fibrillation is an independent predictor of CVA and this association may have important clinical implications in CVA risk stratification. (more…)Polysomnography Remains Standard For Pediatric Obstructive Sleep Apnea Diagnosis
 MedicalResearch.com Interview with:
Ron B. Mitchell, MD
Professor of Otolaryngology and Pediatrics
William Beckner Distinguished Chair in Otolaryngology
Chief of Pediatric Otolaryngology
UT Southwestern and Children's Medical Center Dallas
ENT Clinic Dallas, TX 75207
Medical Research: What is the background for this study? What are the main findings?
Dr. Mitchell: The “gold standard” for the diagnosis of and quantification of obstructive sleep apnea (OSA) is polysomnography (PSG or a ‘sleep study’). However, the majorities of T&A procedures are done without PSG and are based on a clinical diagnosis. This is because PSG is expensive, requires overnight observation and is often unavailable. It is important to diagnose and quantify OSA as it allows for surgical planning and predicts the need and type of treatment after surgery.
We used data from the Childhood Adenotonsillectomy (CHAT) study; a large multicenter
trial (RCT), to look at the ability of clinical parameters to predict the severity of obstructive sleep apnea in children scheduled for a T&A.
The main findings of the study are that certain clinical parameters such as obesity and African American race as well as high scores on certain validated questionnaires (such as the pediatric sleep questionnaire- PSQ) are associated, but cannot predict OSA severity. PSG remains the only way to measure objectively the severity of OSA.
(more…)
MedicalResearch.com Interview with:
Ron B. Mitchell, MD
Professor of Otolaryngology and Pediatrics
William Beckner Distinguished Chair in Otolaryngology
Chief of Pediatric Otolaryngology
UT Southwestern and Children's Medical Center Dallas
ENT Clinic Dallas, TX 75207
Medical Research: What is the background for this study? What are the main findings?
Dr. Mitchell: The “gold standard” for the diagnosis of and quantification of obstructive sleep apnea (OSA) is polysomnography (PSG or a ‘sleep study’). However, the majorities of T&A procedures are done without PSG and are based on a clinical diagnosis. This is because PSG is expensive, requires overnight observation and is often unavailable. It is important to diagnose and quantify OSA as it allows for surgical planning and predicts the need and type of treatment after surgery.
We used data from the Childhood Adenotonsillectomy (CHAT) study; a large multicenter
trial (RCT), to look at the ability of clinical parameters to predict the severity of obstructive sleep apnea in children scheduled for a T&A.
The main findings of the study are that certain clinical parameters such as obesity and African American race as well as high scores on certain validated questionnaires (such as the pediatric sleep questionnaire- PSQ) are associated, but cannot predict OSA severity. PSG remains the only way to measure objectively the severity of OSA.
(more…)Sleep Apnea Predicts Atrial Fibrillation after CABG
MedicalResearch.comInterview with: Amro Qaddoura BHSc Research Student of Adrian Baranchuk, MD Department of Medicine, Queen's University, Kingston, Ontario, Canada MedicalResearch: What is the...
CPAP May Improve Depression In Patients With Sleep Apnea
 MedicalResearch.com Interview with:
Dr. Marcus Povitz MD
Department of Community Health Sciences
University of Calgary, Calgary, Alberta, Canada
Adjunct Professor and Clinical Fellow
Western University Department of Medicine,
Western University, London, Ontario, Canada
Medical Research: What is the background for this study? What are the main findings?
Dr. Povitz: Both depression and obstructive sleep apnea are important causes of illness and have overlapping symptoms. Both feature poor quality sleep, difficulty with concentration and memory as well as daytime sleepiness or fatigue. Previous research showed that depression is common in individuals with sleep apnea, but studies investigating the effect of treating sleep apnea on depressive symptoms have had conflicting results. Our study combined the results of all randomized controlled trials of participants who were treated for sleep apnea with CPAP or mandibular advancement devices where symptoms of depression were measured both before and after treatment. We found that in studies of individuals without a lot of symptoms of depression there was still a small improvement in these symptoms after treatment with CPAP or mandibular advancement device. In 2 studies of individuals with more symptoms of depression there was a large improvement in symptoms of depression.
(more…)
MedicalResearch.com Interview with:
Dr. Marcus Povitz MD
Department of Community Health Sciences
University of Calgary, Calgary, Alberta, Canada
Adjunct Professor and Clinical Fellow
Western University Department of Medicine,
Western University, London, Ontario, Canada
Medical Research: What is the background for this study? What are the main findings?
Dr. Povitz: Both depression and obstructive sleep apnea are important causes of illness and have overlapping symptoms. Both feature poor quality sleep, difficulty with concentration and memory as well as daytime sleepiness or fatigue. Previous research showed that depression is common in individuals with sleep apnea, but studies investigating the effect of treating sleep apnea on depressive symptoms have had conflicting results. Our study combined the results of all randomized controlled trials of participants who were treated for sleep apnea with CPAP or mandibular advancement devices where symptoms of depression were measured both before and after treatment. We found that in studies of individuals without a lot of symptoms of depression there was still a small improvement in these symptoms after treatment with CPAP or mandibular advancement device. In 2 studies of individuals with more symptoms of depression there was a large improvement in symptoms of depression.
(more…)Snoring During Twenties May Be Predictive of Sleep Apnea in Forties
MedicalResearch.com Interview with: Dr. Swati Gulati, MD Internal Medicine John H. Stroger Hospital of Cook County Chicago, IL Medical Research: What are the...
CHEST 2014: Obstructive Sleep Apnea Linked To Cognitive Difficulties in Postmenopausal Women
 MedicalResearch.com Interview with:
Chitra Lal, MD. Assistant Professor
Medical University of South Carolina
Medical Research: What are the main findings of the study?
Dr. Lal: We studied the prevalence of cognitive problems in early postmenopausal women (age 45-60 years) with obstructive sleep apnea syndrome (OSAS+) and without obstructive sleep apnea syndrome (OSAS-) using a questionnaire called the Mail-In Cognitive Function Screening Instrument (MCFSI).
We found that the mean MCFSI scores after adjusting for depression were significantly higher in obstructive sleep apnea syndrome+ then the OSAS- group, indicating more self-reported cognitive difficulty in OSAS+ women
(more…)
MedicalResearch.com Interview with:
Chitra Lal, MD. Assistant Professor
Medical University of South Carolina
Medical Research: What are the main findings of the study?
Dr. Lal: We studied the prevalence of cognitive problems in early postmenopausal women (age 45-60 years) with obstructive sleep apnea syndrome (OSAS+) and without obstructive sleep apnea syndrome (OSAS-) using a questionnaire called the Mail-In Cognitive Function Screening Instrument (MCFSI).
We found that the mean MCFSI scores after adjusting for depression were significantly higher in obstructive sleep apnea syndrome+ then the OSAS- group, indicating more self-reported cognitive difficulty in OSAS+ women
(more…)Sleep Apnea Increases Risk of Atrial Fibrillation After Bypass Surgery
 MedicalResearch.com Interview with:
Adrian Baranchuk MD FACC FRCPC
Associate Professor of Medicine
Director, EP Training Program Queen's University
Kingston, Ontario, Canada
Medical Research: What are the main findings of the study?
Dr. Baranchuk: In this study, we investigated whether obstructive sleep apnea increases the risk of atrial fibrillation after coronary artery bypass surgery. We found the risk to increase by approximately two-fold for patients with obstructive sleep apnea, suggesting that this disease is a strong predictor of atrial fibrillation after coronary artery bypass surgery.
We also found that the risk increases in patients with more severe obstructive sleep apnea.
This is an important association to explore since atrial fibrillation after coronary artery bypass surgery increases patient mortality, the risk of stroke, hospital stay, healthcare costs, and has substantial burden on patients and their families. It is also a common complication of the surgery, occurring in up to half of the patients. Knowing which factors increase its risk gives us a better understanding of how to manage it and mitigate its negative consequences.
(more…)
MedicalResearch.com Interview with:
Adrian Baranchuk MD FACC FRCPC
Associate Professor of Medicine
Director, EP Training Program Queen's University
Kingston, Ontario, Canada
Medical Research: What are the main findings of the study?
Dr. Baranchuk: In this study, we investigated whether obstructive sleep apnea increases the risk of atrial fibrillation after coronary artery bypass surgery. We found the risk to increase by approximately two-fold for patients with obstructive sleep apnea, suggesting that this disease is a strong predictor of atrial fibrillation after coronary artery bypass surgery.
We also found that the risk increases in patients with more severe obstructive sleep apnea.
This is an important association to explore since atrial fibrillation after coronary artery bypass surgery increases patient mortality, the risk of stroke, hospital stay, healthcare costs, and has substantial burden on patients and their families. It is also a common complication of the surgery, occurring in up to half of the patients. Knowing which factors increase its risk gives us a better understanding of how to manage it and mitigate its negative consequences.
(more…)Sleep Apnea Predisposes To Impaired Brain Blood Flow With Physical Activity
 MedicalResearch.com Interview with:
Paul M. Macey, Ph.D.
Assistant Professor in Residence
Associate Dean for Information Technology and Innovations,
Chief Innovation Officer UCLA School of Nursing and Brain Research Institute
Medical Research: What are the main findings of the study?
Dr. Macey: People with sleep apnea are less able to control the blood flowing to their brain, in particular when they grip tightly, or have their foot put in cold water. We measured changes in blood flowing through the brain using an MRI scanner while people gripped hard, had their foot placed in cold water, and breathed out hard into a tube with a very small hole in it. These activities all lead to more blood flowing to the brain in healthy people, which probably helps protect the cells from being starved of blood and oxygen. However, people with sleep apnea send less blood that the healthy participants during the gripped and cold foot activities.
A further important finding is that women with sleep apnea are worse off than men. The female patients showed much weaker blood flow than the males, even accounting for normal differences between men and women.
(more…)
MedicalResearch.com Interview with:
Paul M. Macey, Ph.D.
Assistant Professor in Residence
Associate Dean for Information Technology and Innovations,
Chief Innovation Officer UCLA School of Nursing and Brain Research Institute
Medical Research: What are the main findings of the study?
Dr. Macey: People with sleep apnea are less able to control the blood flowing to their brain, in particular when they grip tightly, or have their foot put in cold water. We measured changes in blood flowing through the brain using an MRI scanner while people gripped hard, had their foot placed in cold water, and breathed out hard into a tube with a very small hole in it. These activities all lead to more blood flowing to the brain in healthy people, which probably helps protect the cells from being starved of blood and oxygen. However, people with sleep apnea send less blood that the healthy participants during the gripped and cold foot activities.
A further important finding is that women with sleep apnea are worse off than men. The female patients showed much weaker blood flow than the males, even accounting for normal differences between men and women.
(more…)Sleep Apnea May Be Improved By Moderate Calorie Restriction
CPAP Effective In Elderly Sleep Apnea Patients
- 1
- 2