MedicalResearch.com Interview with:
Annick Desjardins, M.D., F.R.C.P.C.
Associate Professor of Neurology
Associate Professor of Neurosurgery
Director of Clinical Research
The Preston Robert Tisch Brain Tumor Center at Duke
Duke University School of Medicine
Durham, NC 27710
MedicalResearch.com: What is the background for this study? What are the main findings?
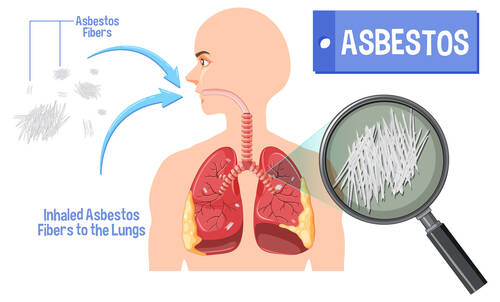
Response: The poliovirus receptor (CD155) is an onco-fetal cell adhesion molecule with widespread expression in all solid tumors and particularly in primary CNS tumors (adult and pediatric).
Recombinant nonpathogenic polio–rhinovirus chimera (PVSRIPO) was generated by replacing a critical piece of the genetic information from the Sabin type 1 polio vaccine, making PVSRIPO incapable of harming or killing normal brain cells, but toxic/lethal in cancer cells. In preclinical models, it has been demonstrated that the infection of tumor cells, leads to the release of danger signals, which triggers a recruitment of dendritic/CD4/CD8 T cells and a destruction of tumor cells by anti-tumor T cells.
The manuscript reports the results of the phase 1 trial of PVSRSIPO in recurrent WHO grade IV malignant glioma patients. Adult patients with recurrence of a single glioblastoma lesion, 1-5.5cm in dimension, in a non-eloquent area of the brain, were enrolled on study. PVSRIPO is injected slowly over 6.5 hours directly into the tumor via a small catheter inserted via a small bur hole. Once intratumoral injection is completed, the catheter is removed and patients are observed for localized tumor inflammation, followed by tumor contraction. A total of 61 patients were treated on study, 9 patients in a dose escalation phase and 52 in a dose expansion phase. Side effects observed were in relation to the localized inflammation of the tumor and depending on the cerebral functions in close proximity to the tumor: headaches, visual field changes, hemiparesis, etc.
One patient experienced a brain hemorrhage at the time of catheter removal, which triggered right sided weakness and aphasia. The patient remained alive 57.5 months after PVSRIPO infusion at data cutoff of March 20
th, 2018. Two on-study death were observed, a patient died from cerebral edema and seizures, which was later found to be due to tumor progression, and one patient died from the complications of an intracranial hemorrhage while receiving anticoagulation and bevacizumab.
The median overall survival among all 61 patients who received PVSRIPO was 12.5 months (95% CI, 9.9 to 15.2), comparatively to 11.3 months (95% CI, 9.8 to 12.5) in a historical control group of patients treated at Duke and who would have met eligibility on trial, would have the trial been available to them.
At 24 months, the survival plateaued in patients treated with PVSRIPO with an overall survival rate of 21% (95% CI, 11 to 33) at 24 months and 36 months in PVSRIPO treated patients, while overall survival in the historical control group continued to decline, with an overall survival rates of 14% (95% CI, 8 to 21) at 24 months and 4% (95% CI, 1 to 9) at 36 months in the historical control group.
(more…)





 Response: LENVIMA (lenvatinib), discovered and developed by Eisai, is an orally available multiple receptor tyrosine kinase inhibitor that inhibits the kinase activities of vascular endothelial growth factor (VEGF) receptors VEGFR1 (FLT1), VEGFR2 (KDR), and VEGFR3 (FLT4). LENVIMA inhibits other kinases that have been implicated in pathogenic angiogenesis, tumor growth, and cancer progression in addition to their normal cellular functions, including fibroblast growth factor (FGF) receptors FGFR1-4, the platelet derived growth factor receptor alpha (PDGFRα), KIT, and RET.
LENVIMA is approved in combination with everolimus for the treatment of patients with advanced renal cell carcinoma (RCC) following one prior anti-angiogenic therapy. The approved starting dose for LENVIMA is 18 mg daily. The objective of Study 218, a randomized, open-label, Phase 2 trial, was to assess whether the lower starting dose of LENVIMA (14 mg daily) in combination with everolimus (5 mg daily) would provide similar efficacy with an improved safety profile compared to the FDA-approved starting dose of LENVIMA (18 mg daily) plus everolimus (5 mg daily) in patients with advanced renal cell carcinoma (RCC) following prior treatment with an antiangiogenic therapy.
In the US, LENVIMA is also indicated for:
Response: LENVIMA (lenvatinib), discovered and developed by Eisai, is an orally available multiple receptor tyrosine kinase inhibitor that inhibits the kinase activities of vascular endothelial growth factor (VEGF) receptors VEGFR1 (FLT1), VEGFR2 (KDR), and VEGFR3 (FLT4). LENVIMA inhibits other kinases that have been implicated in pathogenic angiogenesis, tumor growth, and cancer progression in addition to their normal cellular functions, including fibroblast growth factor (FGF) receptors FGFR1-4, the platelet derived growth factor receptor alpha (PDGFRα), KIT, and RET.
LENVIMA is approved in combination with everolimus for the treatment of patients with advanced renal cell carcinoma (RCC) following one prior anti-angiogenic therapy. The approved starting dose for LENVIMA is 18 mg daily. The objective of Study 218, a randomized, open-label, Phase 2 trial, was to assess whether the lower starting dose of LENVIMA (14 mg daily) in combination with everolimus (5 mg daily) would provide similar efficacy with an improved safety profile compared to the FDA-approved starting dose of LENVIMA (18 mg daily) plus everolimus (5 mg daily) in patients with advanced renal cell carcinoma (RCC) following prior treatment with an antiangiogenic therapy.
In the US, LENVIMA is also indicated for: