Author Interviews, Cannabis, Ophthalmology, Race/Ethnic Diversity, Social Issues / 09.11.2020
Ophthalmology: Identifying Racial and Socioeconomic Disparities in Eye Health
MedicalResearch.com Interview with:
Joshua Uhr MD
Ophthalmologist
Philadelphia, PA
MedicalResearch.com: What is the background for this study?
Response: Disparities in American society have been at the forefront of the public consciousness in recent months. As part of the larger discussion about inequality, disparities in health outcomes have received much attention. In light of the renewed recognition that these disparities are stark and widespread, we felt it important to evaluate disparities in our own field, ophthalmology.
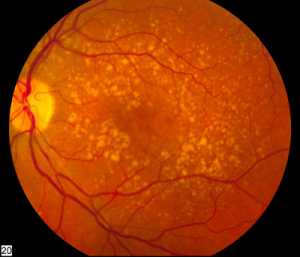
Previous studies have shown disparate outcomes for individual eye conditions, such as glaucoma, cataract, and retinal detachment. Although the common and relevant endpoint of these is visual impairment, few prior studies have examined disparities in visual impairment more broadly. Our aim was to provide an updated analysis of disparity in visual impairment among adults in the United States based on race and socioeconomic status. (more…)




 Prof. FAN Zhiyong PhD
University of California, Irvine
HKUST School of Engineering
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: According to the report of The World Health Organization, there are over 252 million people suffering from visual impairment globally and 15 million of them are difficult to cure by conventional medical methods. However, today, even the best bionic eyes have only 200 clinical trials, less than 1 ppm of all the patients, mainly due to their poor performance and high cost. The huge gap in supply and demand triggers the study of bionic eyes with performance comparable to human eyes. One important reason for their poor performance is the mismatch in shape between the flat bionic eyes and concave sclera. To protect the soft tissue in eyes from being damaged by the bionic surface, the implanted bionic eyes have to be small. This has limited the sensing area and further the electrodes number, and finally yielded poor image sensing characters with low resolution and narrow field-of-view.
In this work, we are trying to achieve high performance image sensing by biomimeticing human eyes. The high-density NWs are well aligned and embedded in a hemispherical template to serve as retina. The conformal attachment of bionic eyes with sclera enables the large sensing area and wide visual angle. In addition, each individual high-density nanowires can potentially work as an individual pixel. By addressing these challenges, our device design has huge potential to improve the image sensing performance of bionic eyes.
Prof. FAN Zhiyong PhD
University of California, Irvine
HKUST School of Engineering
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: According to the report of The World Health Organization, there are over 252 million people suffering from visual impairment globally and 15 million of them are difficult to cure by conventional medical methods. However, today, even the best bionic eyes have only 200 clinical trials, less than 1 ppm of all the patients, mainly due to their poor performance and high cost. The huge gap in supply and demand triggers the study of bionic eyes with performance comparable to human eyes. One important reason for their poor performance is the mismatch in shape between the flat bionic eyes and concave sclera. To protect the soft tissue in eyes from being damaged by the bionic surface, the implanted bionic eyes have to be small. This has limited the sensing area and further the electrodes number, and finally yielded poor image sensing characters with low resolution and narrow field-of-view.
In this work, we are trying to achieve high performance image sensing by biomimeticing human eyes. The high-density NWs are well aligned and embedded in a hemispherical template to serve as retina. The conformal attachment of bionic eyes with sclera enables the large sensing area and wide visual angle. In addition, each individual high-density nanowires can potentially work as an individual pixel. By addressing these challenges, our device design has huge potential to improve the image sensing performance of bionic eyes.