Author Interviews, Mental Health Research, Psychological Science / 01.12.2020
Mental and Physical Health Suffer In Recently Divorced
MedicalResearch.com Interview with:
Gert Martin Hald, PhD
Head of Section (Environmental Health), Associate Professor
Department of Public Health, University of Copenhagen
Copenhagen, Denmark
MedicalResearch.com: What is the background for this study?
Response: Basically, much of previous research has investigated mental and physical health of divorcees only after extensive separation periods, which is mandatory in most countries before juridical divorce unless infidelity or violence is involved in the divorce. During the time of data collection (2016-2019), Denmark where data was collected did not require separation periods before granting divorce. This means that as a first, we could investigate the mental and physical health of divorcees within days of them filling for divorce and perhaps better and more accurately pick up well-known adverse effects of mental- and physical health states of divorcees at the time of their divorce. (more…)



 Response: Cohen Veterans Bioscience (CVB) is a non-profit 501(c)(3) research biotech dedicated to fast-tracking the development of diagnostic tests and personalized therapeutics for the millions of Veterans and civilians who suffer the devastating effects of trauma-related and other brain disorders.
To learn about CVB’s research efforts visit
Response: Cohen Veterans Bioscience (CVB) is a non-profit 501(c)(3) research biotech dedicated to fast-tracking the development of diagnostic tests and personalized therapeutics for the millions of Veterans and civilians who suffer the devastating effects of trauma-related and other brain disorders.
To learn about CVB’s research efforts visit 





















 Dr Sarah Myers PhD
Honorary Research Associate
UCL Department of Anthropology
MedicalResearch.com: What is the background for this study?
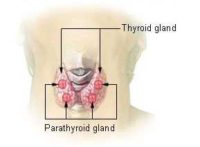
Response: Postnatal or postpartum depression is unfortunately common after giving birth; a figure often quoted is 15%, but some studies have found much higher numbers. Postnatal depression is associated with a range of poorer outcomes for mothers and their infants, and the financial costs of treating maternal mental ill health put health services under considerable strain. Studies have found that providing additional emotional support to at risk mothers, for instance via peer support programmes or regular phone calls with health visitors, can reduce the likelihood of them developing the condition. Therefore, it is really important that we understand the full range of risk factors that put women at greater risk of becoming depressed after giving birth.
There is increasing evidence for a link between inflammation and depression, with factors that trigger an inflammatory immune response also increasing the likelihood of depressive symptoms. The opens up the possibility of finding new risk factors for postnatal depression based on known associations with inflammation.
Dr Sarah Myers PhD
Honorary Research Associate
UCL Department of Anthropology
MedicalResearch.com: What is the background for this study?
Response: Postnatal or postpartum depression is unfortunately common after giving birth; a figure often quoted is 15%, but some studies have found much higher numbers. Postnatal depression is associated with a range of poorer outcomes for mothers and their infants, and the financial costs of treating maternal mental ill health put health services under considerable strain. Studies have found that providing additional emotional support to at risk mothers, for instance via peer support programmes or regular phone calls with health visitors, can reduce the likelihood of them developing the condition. Therefore, it is really important that we understand the full range of risk factors that put women at greater risk of becoming depressed after giving birth.
There is increasing evidence for a link between inflammation and depression, with factors that trigger an inflammatory immune response also increasing the likelihood of depressive symptoms. The opens up the possibility of finding new risk factors for postnatal depression based on known associations with inflammation.