MedicalResearch.com Interview with:
Stewart A. Factor, D.O.
Professor of Neurology
Director of the Movement Disorders Program
Vance Lanier Chair of Neurology
Emory University School of Medicine
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by OFF episodes.
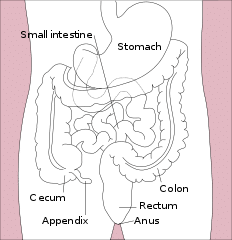
Response: Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disease characterized by motor symptoms, including tremor at rest, rigidity and impaired movement, as well as significant non-motor symptoms, such as cognitive impairment, psychiatric symptoms and autonomic symptoms (i.e. urinary issues, constipation, low blood pressure). It is the second-most common neurodegenerative disease after Alzheimer’s disease and it is predicted that the prevalence of Parkinson’s disease will double by the year 2040. The symptoms of PD are in substantial part, due to loss of dopamine nerve cells in the brain. The current standard of care for PD includes replacing the dopamine loss by the use of oral carbidopa/levodopa. Levodopa is a precursor of dopamine, converted in the brain.
OFF episodes have been a significant unmet need in Parkinson’s disease since the emergence of levodopa. Initially, levodopa controls PD symptoms in a continuous fashion throughout the day. With time the response becomes less predictable and patients experience a re-emergence or worsening of PD symptoms. These episodes are what we mean by OFF episodes. OFF episodes can be characterized, in part, by re-emergence of motor symptoms including tremor, stiffness or slowed movement that can happen at any point during the day. OFF episodes typically begin within the first five years of treatment and occur at the end of a dose. This is referred to as end of dose failure or wearing off. Within the first four to six years after diagnosis, regardless of disease severity, up to 60 percent of people with PD experience OFF episodes. With time these episodes become longer, more severe and disabling, more frequent and less predictable as PD progresses. They can take up more than half the day
OFF episodes may alter a persons’ ability to perform everyday activities by slowing or even precluding their completion. The result is significant burden and distress for people living with Parkinson’s disease (PD) and their care partners.
CTH-300 was a Phase 3, 12-week, randomized, double-blind, placebo-controlled, parallel group, study examining the efficacy, safety and tolerability of apomorphine hydrochloride sublingual film (KYNMOBI) in people with levodopa-responsive PD complicated by OFF episodes. The primary endpoint was a mean change in the score from pre-dose in the Movement Disorder Society Unified Parkinson's Disease Rating Scale (MDS-UPDRS) Part III Motor Examination at 30 minutes after dosing at the 12-week visit of the maintenance treatment phase. The key secondary endpoint was the percentage of people with PD with a patient-rated full ON (or best) response within 30 minutes at the 12-week visit of the maintenance treatment phase.
(more…)