MedicalResearch.com Interview with:
Norman Kleiman, PhD, MS
Department of Environmental Health Sciences
Mailman School of Public Health
Columbia University, New York, NY
MedicalResearch.com: What is the background for this study?
Response: The 1986 Chornobyl nuclear disaster caused the evacuation of 300,000 persons from the cities and villages surrounding the nuclear power plant complex. Pets and belongings were left behind, and the Soviet authorities ordered all animals within the Chornobyl Exclusion Zone killed. Some dogs evaded destruction, and some 300+ descendants of these animals live primarily at two locations today, immediately surrounding the Nuclear Power Plant (NPP) complex and about 10 km away in Chornobyl city. What is relatively unknown to the general public is that Chornobyl is not a desolate, abandoned wasteland. Some thousands of individuals work there every day in continuing cleanup activities and at two new fuel reprocessing facilities built near the damaged reactor. These areas have been substantially remediated, and the average radiation levels are relatively modest. The dogs, which, while feral, are accustomed to human interaction, live near the workers and are not currently exposed to high radiation levels. In contrast to lower radiation levels, there is a toxic mixture of heavy metals, organics, pesticides, and unknown chemicals left over from years’ long cleanup efforts and the decay of a large former military-industrial complex at the NPP.
Since 2016, the NPP authorities have brought in teams of veterinarians and volunteers to spay, neuter, and vaccinate the dogs to protect the workers and deal with a growing population. At the same time, some scientists joined the teams to obtain various kinds of biospecimens (hair, urine, feces, blood, saliva, parasites) to examine the animals’ health and learn how this toxic environment may have affected them or their offspring. Since dogs are human companion animals and live closely with us, any information we learn about health risks to the dogs may be relevant to protecting human workers and inform us about the kinds of health risks posed by ecological and environmental disasters in the future.
(more…)










 Jayant S Vaidya MBBS MS DNB FRCS PhD
Professor of Surgery and Oncology,
Scientific Director, Clinical Trials Group,
Division of Surgery and Interventional Science,
University College London
Whittington Health - Clinical Lead for Breast Cancer
Royal Free Hospital
University College London Hospital
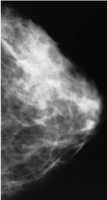
MedicalResearch.com: What is the background for this study? What are the main findings?
Prof. Vaidya: TARGIT-A randomised clinical trial (
Jayant S Vaidya MBBS MS DNB FRCS PhD
Professor of Surgery and Oncology,
Scientific Director, Clinical Trials Group,
Division of Surgery and Interventional Science,
University College London
Whittington Health - Clinical Lead for Breast Cancer
Royal Free Hospital
University College London Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
Prof. Vaidya: TARGIT-A randomised clinical trial (