MedicalResearch.com Interview with:
Heather A. Bimonte-Nelson, Ph.D.
Professor, Barrett Honors Faculty
Department of Psychology
Arizona State University
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The dogma in the field is that the nonpregnant uterus is dormant, and therefore it has not necessarily been of interest to study. Textbooks have described the nonpregnant uterus as “quiescent,” “dormant,” and “useless.” When I was in graduate school studying endocrinology, I read statements in books saying that the sole purpose of the uterus is for gestation.
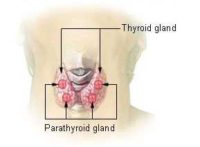
However, all women aging into midlife will experience some type of menopause, and some of these women will undergo surgical menopause via removal of all, or a part of, their reproductive tracts. Research evaluating reproductive tract-brain connections has grown quite a bit in the last few decades. For example, the ovary-brain connection has been focused on quite a bit, and we now know that hormones coming from the ovaries (such as estrogens and progesterone) can affect more than reproduction, and can impact brain functioning. While the uterus-brain connection is not well understood, there is research indicating that the uterus and autonomic nervous system communicate directly.
We also know that hormones released from the ovaries impact the uterus. Therefore, there is a uterus-ovary-brain triad system. This uterus-ovary-brain triad has undergone little scientific investigation for functions outside of reproduction. Given that by age 60 one in three women experience hysterectomy, thereby interrupting this uterus-ovary-brain triad system, we believe it is important to understand the effects of variants of surgical menopause including hysterectomy.
This led to our current evaluation testing multiple variations in surgical menopause using a rat model, where we tested the effects of uterus removal alone (hysterectomy), ovarian removal alone, or uterus plus ovarian removal.
(more…)