Author Interviews, Brigham & Women's - Harvard, Endocrinology, Insomnia, Menopause, Sleep Disorders, Weight Research / 23.03.2021
Poor Sleep During Menopause Linked to Decreased Fat Metabolism
MedicalResearch.com Interview with:
Leilah K. Grant, PhD
Postdoctoral Research Fellow in Medicine
Brigham and Women’s Hospital
Harvard Medical School
MedicalResearch.com: What is the background for this study?
Response: The prevalence of obesity increases in women around the age of menopause which increases the risk of diseases like diabetes and heart disease. Changes in hormones, like estrogen, are thought to contribute to weight gain during menopause, but other common symptoms of menopause such as sleep interruption may also play a role. While short sleep is known to adversely affect metabolism, little is known about the metabolic consequences of the type of sleep disruption most common in menopausal women – increased nighttime awakenings (i.e., sleep interruption) caused by hot flashes, but no change in overall sleep duration. We therefore did this study to see how an experimental model menopause-related sleep interruption would affect metabolic outcomes that may contribute to weight gain. (more…)












 Jennifer Woo Baidal, MD, MPH
Assistant Professor of Pediatrics
Director of Pediatric Weight Management,
Division of Pediatric Gastroenterology, Hepatology, and Nutrition,
Columbia University Medical Center &
New York-Presbyterian Morgan Stanley Children’s Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Childhood obesity prevalence is historically high, with most incident obesity among children occurring before age 5 years. Racial/ethnic and socioeconomic disparities in childhood obesity are already apparent by the first years of life. Latino/Hispanic children in low-income families are at-risk for obesity. Thus, understanding potentially effective ways to prevent childhood obesity, particularly in vulnerable populations, should focus on early life.
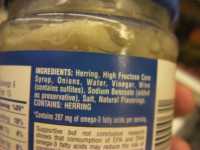
Sugar-sweetened beverage (SSB) consumption is a modifiable risk factor for obesity and is linked to other adverse health outcomes. Maternal SSB consumption in pregnancy and infant sugar-sweetened beverage consumption in the first year of life are linked to later childhood obesity.
We sought to describe beverage consumption in a modern cross-sectional cohort of 394 low-income, Latino families, and to examine the relationship of parental attitudes toward sugar-sweetened beverages with parental and infant SSB consumption.
Jennifer Woo Baidal, MD, MPH
Assistant Professor of Pediatrics
Director of Pediatric Weight Management,
Division of Pediatric Gastroenterology, Hepatology, and Nutrition,
Columbia University Medical Center &
New York-Presbyterian Morgan Stanley Children’s Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Childhood obesity prevalence is historically high, with most incident obesity among children occurring before age 5 years. Racial/ethnic and socioeconomic disparities in childhood obesity are already apparent by the first years of life. Latino/Hispanic children in low-income families are at-risk for obesity. Thus, understanding potentially effective ways to prevent childhood obesity, particularly in vulnerable populations, should focus on early life.
Sugar-sweetened beverage (SSB) consumption is a modifiable risk factor for obesity and is linked to other adverse health outcomes. Maternal SSB consumption in pregnancy and infant sugar-sweetened beverage consumption in the first year of life are linked to later childhood obesity.
We sought to describe beverage consumption in a modern cross-sectional cohort of 394 low-income, Latino families, and to examine the relationship of parental attitudes toward sugar-sweetened beverages with parental and infant SSB consumption.