Author Interviews, Brigham & Women's - Harvard, JAMA, Orthopedics, Osteoporosis, Surgical Research / 15.05.2019
Roux-en-Y Gastric Bypass Linked to More Hip Fractures
MedicalResearch.com Interview with:
Elaine W. Yu, MD, MMSc
Assistant Professor, Harvard Medical School
Director, Bone Density Center
Endocrine Unit, Massachusetts General Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
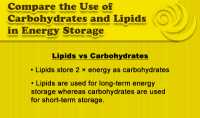
Response: Roux-en-Y gastric bypass (RYGB) is a popular surgical weight loss procedure. We have previously shown that gastric bypass leads to rapid high-turnover bone loss.
Bariatric procedures are being increasingly performed in older adults, and the clinical consequences of gastric bypass-associated skeletal changes in this vulnerable population have been unclear to date. Thus, we used Medicare claims data to investigate fracture risk among older adults after gastric bypass, and in comparison to adults who received another bariatric procedure called adjustable gastric banding (AGB), which is thought to have fewer negative bone effects.
In our analysis, we found that patients undergoing Roux-en-Y gastric bypass were 73% more likely to fracture than those undergoing AGB. Importantly, we found that hip fracture risk increased nearly 180% after RYGB, and that fracture rates in patients aged 65 or older were similar to the overall group. (more…)