Author Interviews, Brigham & Women's - Harvard, Cognitive Issues, Social Issues / 27.02.2020
Widowhood Exacerbates Cognitive Decline in Alzheimer’s Disease
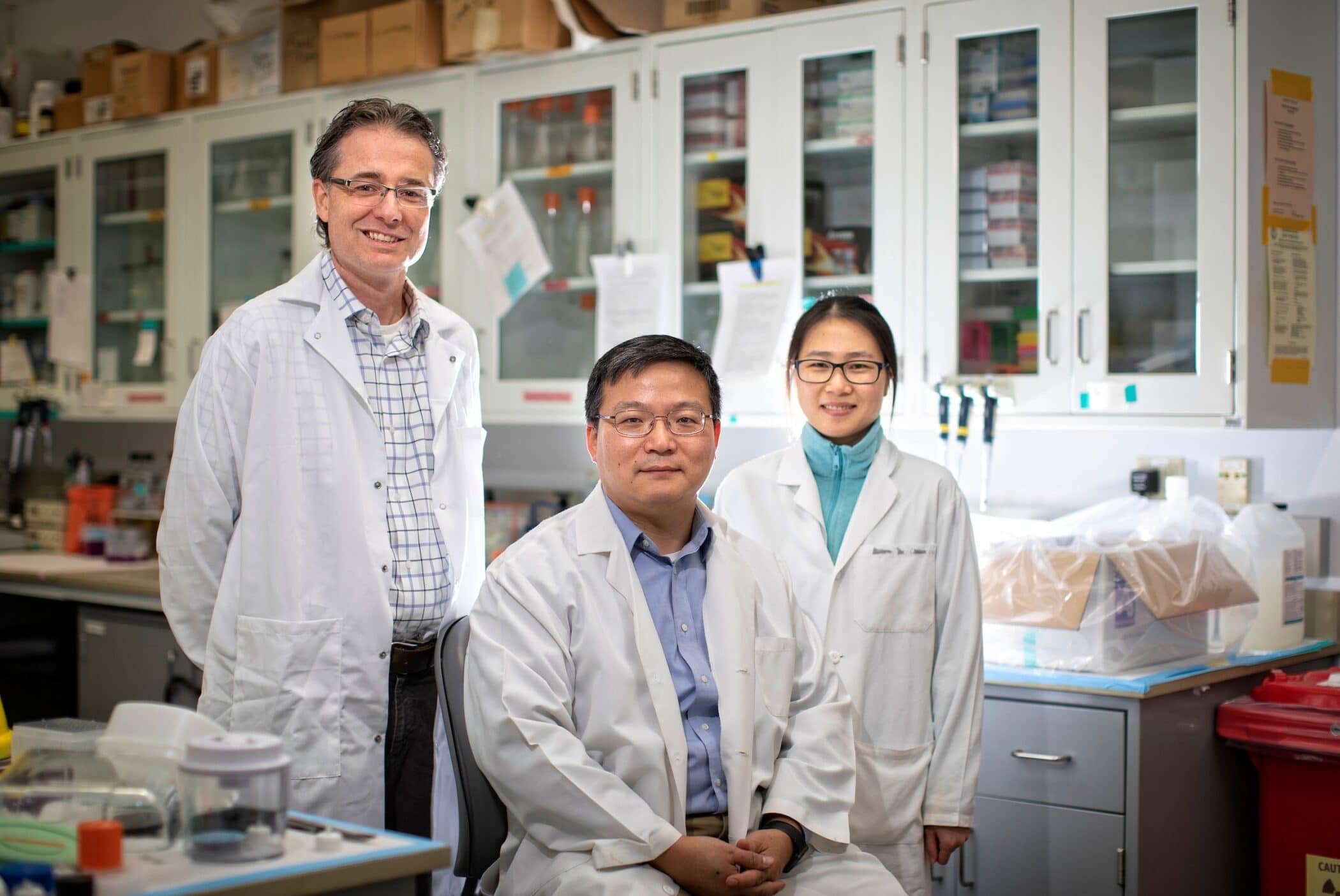
MedicalResearch.com Interview with:
Nancy J. Donovan, M.D.
Chief, Division of Geriatric Psychiatry
Brigham and Women’s Hospital
Assistant Professor of Psychiatry
Harvard Medical School
Boston, MA 02115
MedicalResearch.com: What is the background for this study?
Response: Prior research has shown that widowed older adults are more likely to experience cognitive decline than those who are married. However, there have been no prior studies of widowhood as a risk factor for cognitive decline due to Alzheimer’s disease, the most common cause of severe cognitive impairment.
(more…)