Alzheimer's - Dementia, Author Interviews, Diabetes, JAMA, Weight Research / 09.04.2025
Study Suggests GLP-1 Obesity Drugs Associated with Lower Risk of Dementia
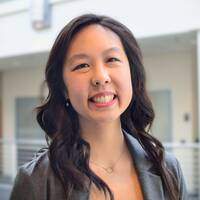
MedicalResearch.com Interview with:
Dr. Catriona Reddin MD
Fourth year Specialist Registrar in Geriatric Medicine and
an Irish Clinical Academic Training (ICAT) fellow
University Hospital Galway, Galway, Ireland
MedicalResearch.com: What is the background for this study?
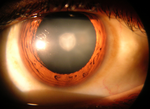
Response: Dementia is a leading cause of disability globally, which is projected to affect approximately 75 million people by 2030. Diabetes mellitus is a risk factor for dementia, it was unclear if glucose lower therapies reduce the risk of dementia. The research, a systematic review and meta-analysis of 26 clinical trials involving over 160,000 participants, found that while most glucose-lowering therapies were not significantly associated with a reduction in dementia risk, one class of drugs—GLP-1Ras—was linked to a significant reduction.
(more…)