MedicalResearch.com Interview with:
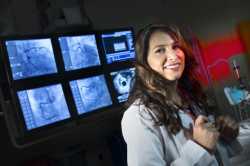
 Dr. Kyla M Lara
Dr. Kyla M Lara
Icahn School of Medicine at Mount Sinai
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: This was the first study to evaluate whether dietary patterns of black and white adults living in the United States were associated with developing heart failure. We’re hearing a lot in the news about specific diets like low-fat, high protein, low carb, and other diets that decrease cardiovascular risk. We would love it, as physicians, if we could prescribe a specific diet to limit cardiovascular risk in our patients. I’m really excited about our study because instead of examining patterns of what we already know are healthy, we looked at foods people were regularly consuming in the United States and developed dietary patterns from this. This study is similar to other work we have done with stroke and heart attack.
We used data from the NIH funded REGARDS study, also known as the Reasons for Geographic and Racial Differences in Stroke. More than 30,000 white and African-American adults were recruited from 2003-2007. From this group, we studied over 18,000 adults who successfully completed a dietary assessment called the Food Frequency Questionnaire. This was a really great group to study because people who live in this particular geographic area of the Southeastern United States, also known as the stroke belt, suffer from a higher risk of death from stroke. It’s extremely important for us to better understand the major risk factors that contribute to this and also cardiovascular disease.
We used statistical techniques to derive 5 dietary patterns based on the types of foods participants tended to eat.
• Convenience - Mexican and Chinese food, mixed dishes (both meat and bean)
• Sweets - added fats, bread, chocolate, desserts, sweet breakfast foods
• Southern - added fats, fried food, organ and processed meat, fatty milk
• Alcohol/Salads - beer, wine, liquor, green leafy vegetables, salad dressings, nuts and seeds, coffee
• Plant Based- fruit, vegetables, fruit juice, cereal, fish, poultry
Each participant received a score for each pattern that reflected how closely their diet resembled that dietary pattern. This approach reflects the real world and how people eat.
Over the 3135 days (8.6 years) of median follow up, 594 participants were hospitalized for incident HF. Greatest adherence to the plant-based dietary pattern during the study period was associated with a 28% risk reduction of developing heart failure.
(more…)