Author Interviews, Biomarkers, Heart Disease, JAMA / 05.11.2018
New Biomarker Allows ‘Liquid Biopsy’ of Heart Muscle
MedicalResearch.com Interview with:
Robin M. Shaw, MD, PhD
Wasserman Foundation Chair in Cardiology
in honor of S. Rexford Kennamer MD
Division of Cardiology, Smidt Heart Institute
Department of Medicine, Cedars-Sinai Medical Center,
Division of Cardiology, Department of Medicine
University of California,
Los Angeles, California
MedicalResearch.com: What is the background for this study? What are the main findings?
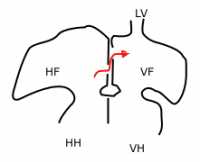
Response: At present, doctors do not have a clinical tool that assesses the biochemical health of heart muscle. Biomarkers are available that tests the amount of fluid in the heart, and whether a heart is overloaded (which can be resolved with diuretics). However, we don’t have biomarkers that assess the state of heart muscle itself. As a result, doctors can use biomarkers to determine whether, when a patient has trouble breathing, there is heart failure present.
However, biomarkers do not work when the patient does not have symptoms or when we already know the patient has heart failure and are trying to make clinical management decisions about the condition.
Current biomarkers also don’t work to assess the health of the heart before symptoms develop which is to detect cellular changes in muscle before overall heart function is impaired. The new biomarker, CS, address the above unmet needs. CS is based on cBIN1 which is a heart muscle protein that is essential for the heart to both contract and relax. cBIN1 decrease when hearts are stressed such as in heart failure. cBIN1 is also released into the blood stream, so it can be detected from a simple blood draw. CS is determined from the inverse of cBIN1, so low cBIN1 in blood will give a high CS signal. A low cBIN1, or a high CS, indicates failing heart muscle, and an increased likelihood for being admitted to the hospital with acute heart failure within the next twelve months. (more…)



 Dr. Wanpen Vongpatanasin, M.D.
Professor of Medicine
Program Director, Hypertension Fellowship Program
UT Southwestern Medical Center in Dallas
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The new US hypertension guideline places a greater emphasis on out-of-office blood pressure measurement, and maintains that a clinic BP of 130/80 mm Hg is equivalent to the same reading for home BP monitoring or daytime ambulatory BP monitoring. That is based, however, on data from non-US cohorts, primarily from Japanese cohorts and some European populations. None has been studied in the US population until now.
To find out, we analyzed large multi-ethnic studies of primarily young and middle-aged adults in Dallas, Texas, and Durham, N.C., that compared home blood pressure to clinic measurements, using the regression correlation (i.e. regression approach). To confirm the findings, we use another approach called “outcome approach” by determining risks of stroke, MI, and death associated with a clinic systolic blood pressure reading of 130 mmHg from the 3,132 participants in the Dallas study during an 11-year follow up.
Then, we determined the home blood pressure levels that carried the same heart disease risk and stroke risk as the clinic systolic 130 mm Hg reading.
We found that the level of home blood pressure of 130/80 mm Hg actually best correlates with blood pressure taken at the doctor’s office of 130/80 mmHg. This is true for whites, blacks and Hispanic patients in both treated and untreated population.
Dr. Wanpen Vongpatanasin, M.D.
Professor of Medicine
Program Director, Hypertension Fellowship Program
UT Southwestern Medical Center in Dallas
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The new US hypertension guideline places a greater emphasis on out-of-office blood pressure measurement, and maintains that a clinic BP of 130/80 mm Hg is equivalent to the same reading for home BP monitoring or daytime ambulatory BP monitoring. That is based, however, on data from non-US cohorts, primarily from Japanese cohorts and some European populations. None has been studied in the US population until now.
To find out, we analyzed large multi-ethnic studies of primarily young and middle-aged adults in Dallas, Texas, and Durham, N.C., that compared home blood pressure to clinic measurements, using the regression correlation (i.e. regression approach). To confirm the findings, we use another approach called “outcome approach” by determining risks of stroke, MI, and death associated with a clinic systolic blood pressure reading of 130 mmHg from the 3,132 participants in the Dallas study during an 11-year follow up.
Then, we determined the home blood pressure levels that carried the same heart disease risk and stroke risk as the clinic systolic 130 mm Hg reading.
We found that the level of home blood pressure of 130/80 mm Hg actually best correlates with blood pressure taken at the doctor’s office of 130/80 mmHg. This is true for whites, blacks and Hispanic patients in both treated and untreated population.