USPSTF: Evaluates Benefits of Diet and Exercise Counseling for Adults Without Known Heart Disease Risk Factors
MedicalResearch.com Interview with:
Lori Pbert, Ph.D Professor, Department of Population and Quantitative Health Sciences Associate chief of the Division of Preventive and Behavioral Medicine Founder and director of the Center for Tobacco Treatment Research and Training University of Massachusetts Chan Medical School Dr. Pbert joined the U.S. Preventive Services Task Force in January 2019
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Heart attacks and strokes are the number one killer of adults in the United States. Based on the evidence we reviewed, the Task Force found that some people would benefit from counseling interventions to support their cardiovascular health, however the overall benefits are small. For that reason, we continue to recommend that healthcare professionals decide together with their patients who do not have cardiovascular disease risk factors whether counseling interventions on healthy diet and physical activity might help them prevent heart attacks and strokes. This is a C grade recommendation. (more…)
Premature Menopause May Increase Risk of Heart Failure and AFib
MedicalResearch.com Interview with: Jean Shin Department of Family Medicine Korea University College of Medicine Seoul,Republic of Korea
MedicalResearch.com: What is the background for this study?
Response: Younger age at menopause is a possible risk factor for cardiovascular diseases. However, data on the association among premature menopause, age at menopause, and the risk of heart failure and atrial fibrillation are lacking. We aimed to examine the association of premature menopause and age at menopause with the risk of heart failure and atrial fibrillation. (more…)
Precision Genetics Can Identify Specific Causes of Heart Failure
Not All Patients with Heart Failure Benefit from Salt Restriction
USPSTF: Task Force Recommends Against Beta Carotene and Vitamin E to Prevent Heart Disease or Cancer
First-Line Treatment of Type 2 Diabetes: Cardiovascular Outcomes of SGLT-2 Inhibitors vs Metformin
- Cardiovascular disease affects approximately one-third of the population with type 2 diabetes and accounts for 50%–80% of their mortality
- 1 in 10 people in the US has diabetes
Before Initial Acute Coronary Syndrome: Study Finds Statin Therapy Reduced Heart Failure and Mortality
USPSTF Narrows Recommendations for Daily Aspirin Use
More Complications in Pregnancies Conceived by Assisted Reproductive Technology
AFib: BioSig Technologies PURE EP™ System Improves Intracardiac Signaling During Ablation Procedures
MGH Study Finds Infertility Associated with Increased Risk of Heart Failure
Coronary Artery Disease: Women Have Worse Outcomes Following Both Medical and Invasive Treatments
Smartphone Communicates Genetic Risk, Potentially Enhancing Compliance with Heart Medications
COSMOS: First Large Trial of Cocoa Supplement For Heart Disease and Cancer Prevention
Study Helps Explain Why the Less You Exercise The Harder it Becomes
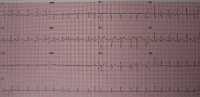
NEJM Study Evaluates Levels of hs Troponin after Cardiac Surgery and Risk of Death
Social isolation and Loneliness Independently Increase Cardiovascular Risk in Women
USPSTF: Screening for Atrial Fibrillation in Adults over 50
COVID 19: Risk of Myocarditis Highest Following Second Vaccine Dose Among Adolescent and Young Adult Males
AHA21: GIRAF Study Results Comparing Anticoagulants and Cognitive Decline in AFib Patients
Penn Study finds Inequities In Access to Heart Procedure TAVR
Study Finds Risk of MI Best Captured By Number of Apolipoprotein B Lipoproteins
Caffeine in Pregnancy: Effects May Differ for Mothers and Offspring
Portable Device Screens for MicroRNAs to Rapidly Detect Heart Attack
Risk of Stroke Acutely Elevated by Episodes of Paroxysmal Atrial Fibrillation
Total Steps Per Day Linked to Risk of Premature Death


NEJM Study Finds Salt Substitute Linked to Reduced Risk of Stroke and Heart Attack
- The salt substitute reduced the risk of stroke by 14%
- The salt substitute reduced the risk of major adverse cardiovascular events by 13%
- The salt substitute reduced the risk of pre-mature death by 12%