Author Interviews, Heart Disease, JAMA, Thyroid Disease, Vanderbilt / 27.01.2019
Link Between Thyroid Function Genetics and Atrial Fibrillation Grows
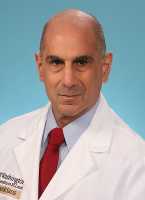
MedicalResearch.com Interview with:
Joe-Elie Salem, MD, PhD
Associate Professor - MCU-PH, Sorbonne Université - INSERM - CIC, Clinical Pharmacology, Cardio-oncology, APHP, La Pitié-Salpêtrière, Paris, France
Adjunct Associate Professor, Vanderbilt University Medical Center, Cardio-oncology
Clinical Pharmacology, Nashville, TN
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: A study by researchers at Vanderbilt University Medical Center has strengthened the link between thyroid function and atrial fibrillation (AF), an irregular heart rhythm that increases the risk of stroke and other heart-related complications.
They phenome-wide association study scanned the medical records of more than 37,000 people for an association between genetically determined variation in thyroid stimulating hormone levels (a measure of thyroid function) and AF risk.
Previous observational studies have found that subclinical hyperthyroidism, an overactive thyroid which does not meet the clinical threshold for diagnosis or treatment, nevertheless can increase the risk of atrial fibrillation. But whether to treat subclinical hypo- or hyperthyroidism to reduce AF risk remains a matter of debate in the medical community. (more…)