MedicalResearch.com Interview with:
Michael E. Belloy, PhD
Department of Neurology and Neurological Sciences
Stanford University, Stanford, California
MedicalResearch.com: What is the background for this study?
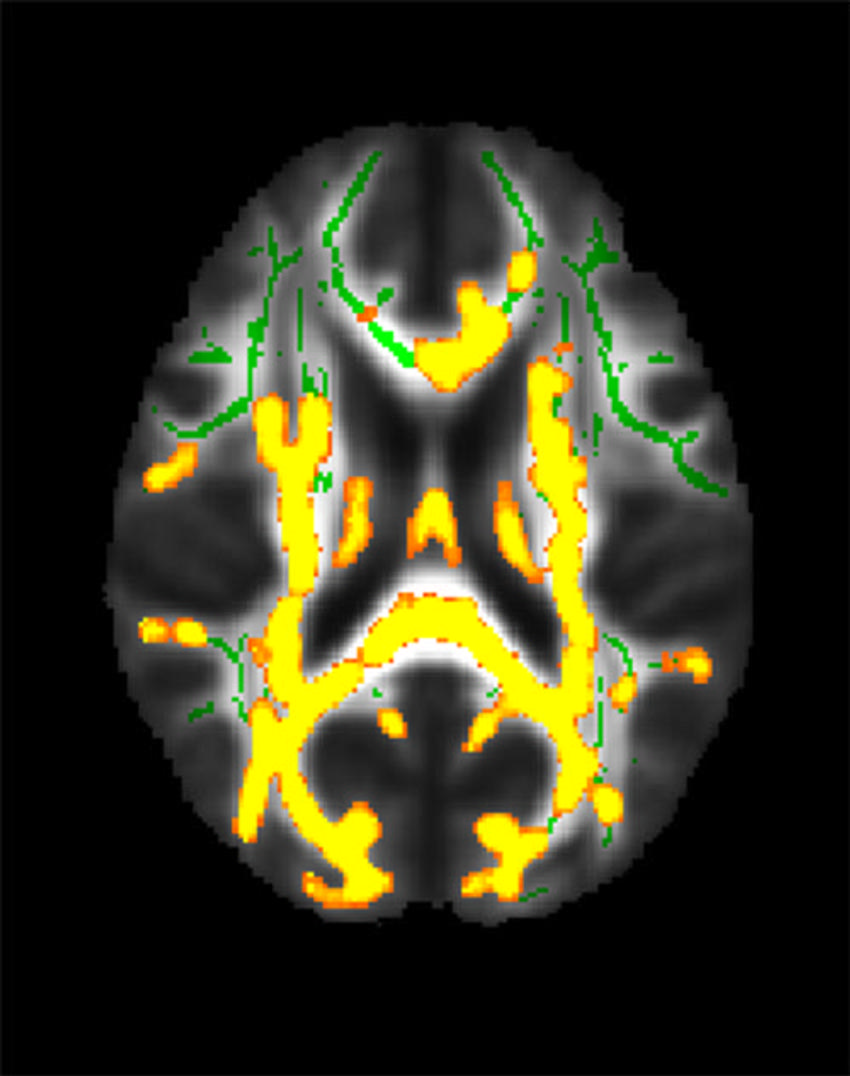
Response: Apolipoprotein E (
APOE)*2 and
APOE*4 are, respectively, the strongest protective and risk-increasing, genetic variants for late-onset Alzheimer disease. As such, one’s
APOE genotype is highly relevant towards clinical trial design and Alzheimer’s disease research. However, most insights so far are focused on the associations of these
APOE genotypes with Alzheimer’s disease risk in non-Hispanic white individuals.
One important aspect of our work is that we really increased sample sizes for non-Hispanic Black, Hispanic, and East Asian individuals, so that we now have better understanding of the associations of
APOE genotypes with Alzheimer’s disease risk in these groups. In complement, we also did the largest investigation to date on the role of ancestry on the associations of
APOE genotypes with Alzheimer’s disease risk. The scale of our study was thus a critical factor in generating novel insights.
(more…)
 In recent years, the field of psychiatric care has undergone a revolutionary transformation. This is because of groundbreaking research that has redefined our understanding of mental health and treatment methodologies.
From innovative therapies to advanced diagnostic tools, transformative research has played a pivotal role in reshaping the landscape of psychiatric care.
In this article, we will explore the key contributions that researchers have made in this field. We will also talk about how their work is influencing the way mental health is approached and treated.
(more…)
In recent years, the field of psychiatric care has undergone a revolutionary transformation. This is because of groundbreaking research that has redefined our understanding of mental health and treatment methodologies.
From innovative therapies to advanced diagnostic tools, transformative research has played a pivotal role in reshaping the landscape of psychiatric care.
In this article, we will explore the key contributions that researchers have made in this field. We will also talk about how their work is influencing the way mental health is approached and treated.
(more…)





 Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.
Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.




 If you've been in a scrape and your noggin took a knock, playing it tough and shaking it off isn't the way to go.
If you've been in a scrape and your noggin took a knock, playing it tough and shaking it off isn't the way to go. 









 One of the most startling aspects of the connection between schizophrenia and substance abuse is the high prevalence of substance use disorders among those with schizophrenia. Studies consistently show that individuals diagnosed with schizophrenia are more likely to engage in substance abuse compared to the general population. This connection can be best demonstrated using the self-medication hypothesis. According to this hypothesis, individuals with schizophrenia may turn to substances as a way to self-medicate or alleviate their distressing symptoms. Imagine dealing with hallucinations or disorganized thoughts—some may use alcohol or drugs to temporarily escape from this internal turmoil.
One of the most startling aspects of the connection between schizophrenia and substance abuse is the high prevalence of substance use disorders among those with schizophrenia. Studies consistently show that individuals diagnosed with schizophrenia are more likely to engage in substance abuse compared to the general population. This connection can be best demonstrated using the self-medication hypothesis. According to this hypothesis, individuals with schizophrenia may turn to substances as a way to self-medicate or alleviate their distressing symptoms. Imagine dealing with hallucinations or disorganized thoughts—some may use alcohol or drugs to temporarily escape from this internal turmoil.
 Lotfi Khemiri
Centre for Psychiatry Research
Stockholm, Sweden
MedicalResearch.com: What is the background for this study?
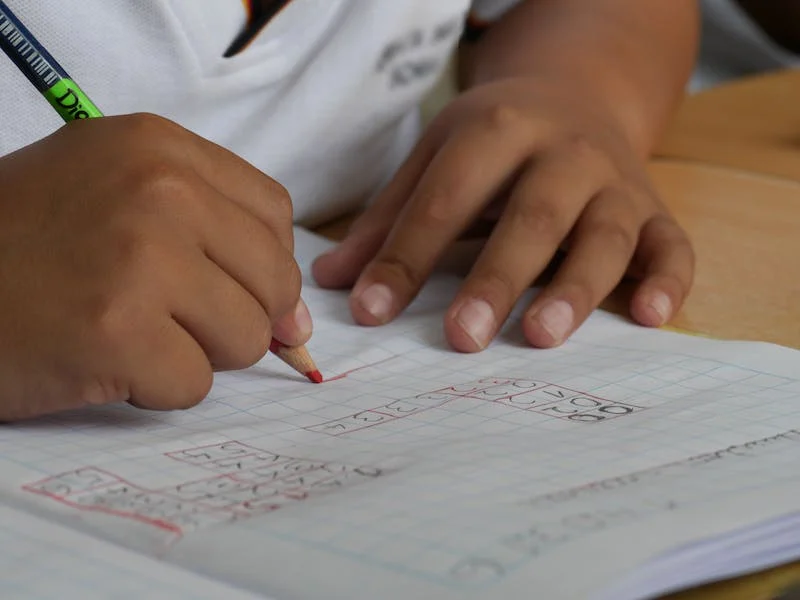
Response: Our study used large-scale national register data in close to 2 million children, and found that parental abuse of both alcohol and drugs are associated with increased risk of intellectual disability in the offspring. Importantly, the risk increase was observed in both mothers and fathers which to the best of our knowledge is a novel finding, and may be explained by both genetic and environmental factors including toxic effects of substance intake on fetal development.
Lotfi Khemiri
Centre for Psychiatry Research
Stockholm, Sweden
MedicalResearch.com: What is the background for this study?
Response: Our study used large-scale national register data in close to 2 million children, and found that parental abuse of both alcohol and drugs are associated with increased risk of intellectual disability in the offspring. Importantly, the risk increase was observed in both mothers and fathers which to the best of our knowledge is a novel finding, and may be explained by both genetic and environmental factors including toxic effects of substance intake on fetal development.