Alzheimer's - Dementia, Author Interviews, Herpes Viruses / 08.01.2025
Hebrew University Study Highlights Interplay of Herpes Virus and Tau in Alzheimer’s Disease
MedicalResearch.com Interview with:
Dr. Or Shemesh PhD
The Harvey M. Krueger Family Center for
Center for Nanoscience and Nanotechnology
School of Pharmacy - Institute for Drug Research
The Hebrew University of Jerusalem
MedicalResearch.com: What is the background for this study?
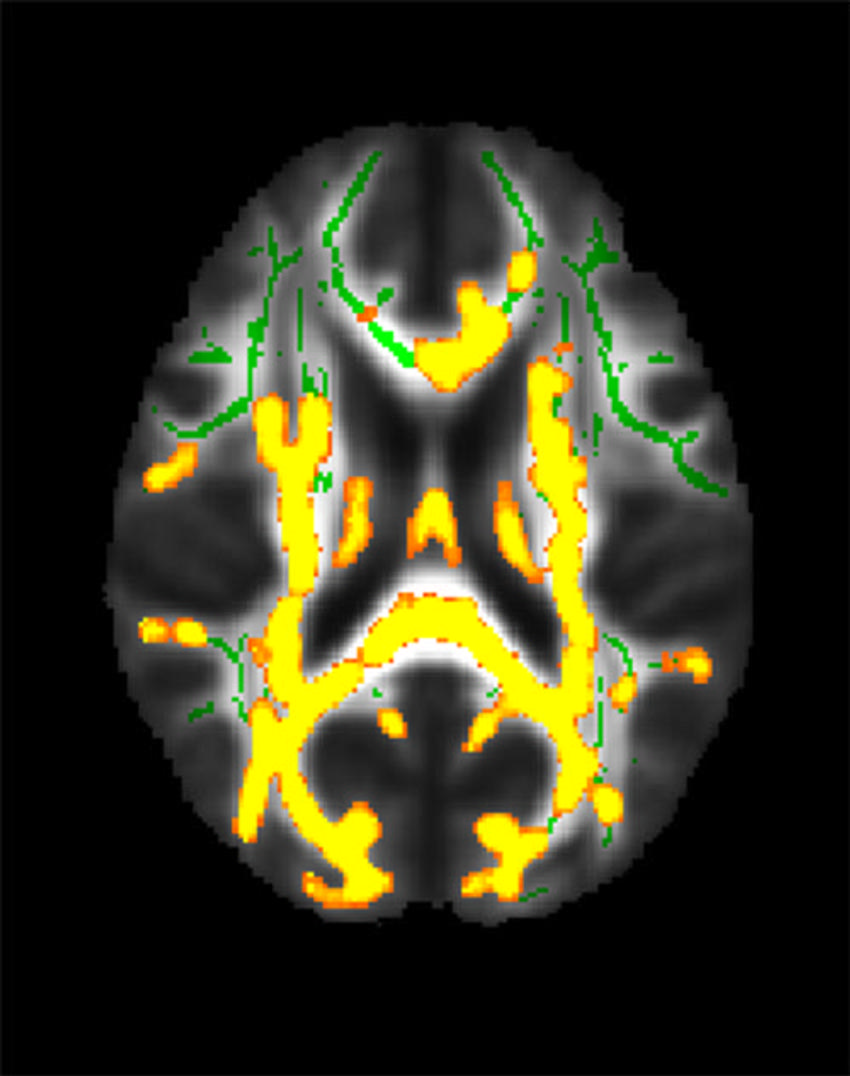
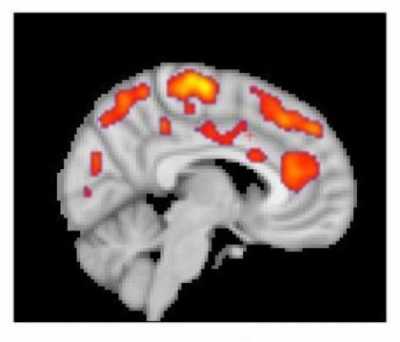
Response: Our study investigated the connection between herpes simplex virus 1 (HSV-1) and Alzheimer's disease (AD) pathologies. We explored how HSV-1 proteins are present in the brains of individuals with AD and examined their interactions with tau, a key protein in AD pathology.
MedicalResearch.com: What are the main findings?
Response: The main finding is that tau, traditionally seen as detrimental, might initially act as a protective response to HSV-1 by reducing neuronal death through an antiviral innate immunity pathway called cGAS-STING . Over time, this (initially beneficial) antiviral response of tau can manifest as the well established tau toxicity in Alzheimer's disease.
(more…)