Author Interviews, Biomarkers, BMJ, Heart Disease / 18.03.2019
Do Elevated Troponins Always Indicate a Heart Attack?
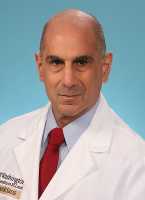
MedicalResearch.com Interview with:
Prof. Nick Curzen BM(Hons) PhD FRCP
Professor of Interventional Cardiology/Consultant Cardiologist
University Hospital Southampton
Southampton
MedicalResearch.com: What is the background for this study?
Response: The commonest blood test now used to assess whether a patient has had a heart attack or not is called high sensitivity troponin (hs trop). The test is supplied with an Upper Limit of Normal, which is based upon results from relatively healthy people. When doctors take the hs trop, they then use this ULN to decide if the patient had has a heart attack.
This study set out to see what the hs trop level is in a large number of patients attending the hospital for any reason, either inpatient or outpatient, in most of whom there was no clinical suspicion of heart attack at all. We therefore took hs trop measurements on 20,000 consecutive patients attending our hospital and having a blood sample for any reason. (more…)