Author Interviews, Heart Disease, JACC, Outcomes & Safety / 17.11.2018
Study Finds Medicare Readmissions Penalties Have Not Increased Mortality from Heart Failure
MedicalResearch.com Interview with:
Teryl K. Nuckols, MD
Vice Chair, Clinical Research
Director, Division of General Internal Medicine
Cedars Sinai
Los Angeles, California
MedicalResearch.com: What is the background for this study?
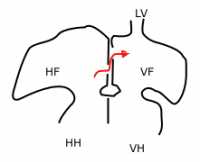
Response: The Medicare Hospital Readmissions Reduction Program (HRRP) penalizes hospitals with increased 30-day readmission rates among seniors admitted with heart failure (HF). Heart failure readmission rates declined markedly following the implementation of this policy. Two facts have raised concerns about whether the HRRP might have also inadvertently increased 30-day heart failure mortality rates.
First, before the policy was implemented, hospitals with higher heart failure readmission rates had lower 30-day HF mortality rates, suggesting that readmissions are often necessary and beneficial in this population. Second, 30-day HF mortality rose nationally after the HRRP was implemented, and the timing of the increase has suggested a possible link to the policy.
Are hospitals turning patients away, putting them at risk of death, or is the increase in heart failure mortality just a coincidence? To answer this question, we compared trends in 30-day HF mortality rates between penalized hospitals and non-penalized hospitals because 30-day HF readmissions declined much more at hospitals subject to penalties under this policy.
(more…)











 Dr. Wanpen Vongpatanasin, M.D.
Professor of Medicine
Program Director, Hypertension Fellowship Program
UT Southwestern Medical Center in Dallas
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The new US hypertension guideline places a greater emphasis on out-of-office blood pressure measurement, and maintains that a clinic BP of 130/80 mm Hg is equivalent to the same reading for home BP monitoring or daytime ambulatory BP monitoring. That is based, however, on data from non-US cohorts, primarily from Japanese cohorts and some European populations. None has been studied in the US population until now.
To find out, we analyzed large multi-ethnic studies of primarily young and middle-aged adults in Dallas, Texas, and Durham, N.C., that compared home blood pressure to clinic measurements, using the regression correlation (i.e. regression approach). To confirm the findings, we use another approach called “outcome approach” by determining risks of stroke, MI, and death associated with a clinic systolic blood pressure reading of 130 mmHg from the 3,132 participants in the Dallas study during an 11-year follow up.
Then, we determined the home blood pressure levels that carried the same heart disease risk and stroke risk as the clinic systolic 130 mm Hg reading.
We found that the level of home blood pressure of 130/80 mm Hg actually best correlates with blood pressure taken at the doctor’s office of 130/80 mmHg. This is true for whites, blacks and Hispanic patients in both treated and untreated population.
Dr. Wanpen Vongpatanasin, M.D.
Professor of Medicine
Program Director, Hypertension Fellowship Program
UT Southwestern Medical Center in Dallas
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The new US hypertension guideline places a greater emphasis on out-of-office blood pressure measurement, and maintains that a clinic BP of 130/80 mm Hg is equivalent to the same reading for home BP monitoring or daytime ambulatory BP monitoring. That is based, however, on data from non-US cohorts, primarily from Japanese cohorts and some European populations. None has been studied in the US population until now.
To find out, we analyzed large multi-ethnic studies of primarily young and middle-aged adults in Dallas, Texas, and Durham, N.C., that compared home blood pressure to clinic measurements, using the regression correlation (i.e. regression approach). To confirm the findings, we use another approach called “outcome approach” by determining risks of stroke, MI, and death associated with a clinic systolic blood pressure reading of 130 mmHg from the 3,132 participants in the Dallas study during an 11-year follow up.
Then, we determined the home blood pressure levels that carried the same heart disease risk and stroke risk as the clinic systolic 130 mm Hg reading.
We found that the level of home blood pressure of 130/80 mm Hg actually best correlates with blood pressure taken at the doctor’s office of 130/80 mmHg. This is true for whites, blacks and Hispanic patients in both treated and untreated population.