Author Interviews, JAMA, Orthopedics, Surgical Research / 03.10.2018
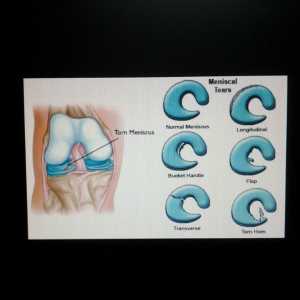
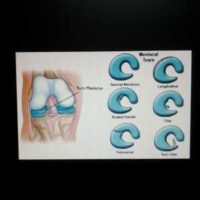
In Non-Locking Meniscal Knee Tears, Physical Therapy May Be As Good As Surgery
MedicalResearch.com Interview with:
 Victor A. van de Graaf, MD
OLVG Ziekenhuis
Amsterdam
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Although meniscal surgeries are among the most frequently performed surgical procedures in orthopedic surgery, until just recently there were hardly any randomized trials proving its superiority over conservative treatment.
In this randomized clinical trial, including 321 patients with non-obstructive (e.g. no locking of the knee joint) meniscal tears, we found physical therapy non-inferior to arthroscopic partial meniscectomy.
(more…)
Victor A. van de Graaf, MD
OLVG Ziekenhuis
Amsterdam
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Although meniscal surgeries are among the most frequently performed surgical procedures in orthopedic surgery, until just recently there were hardly any randomized trials proving its superiority over conservative treatment.
In this randomized clinical trial, including 321 patients with non-obstructive (e.g. no locking of the knee joint) meniscal tears, we found physical therapy non-inferior to arthroscopic partial meniscectomy.
(more…)
 Victor A. van de Graaf, MD
OLVG Ziekenhuis
Amsterdam
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Although meniscal surgeries are among the most frequently performed surgical procedures in orthopedic surgery, until just recently there were hardly any randomized trials proving its superiority over conservative treatment.
In this randomized clinical trial, including 321 patients with non-obstructive (e.g. no locking of the knee joint) meniscal tears, we found physical therapy non-inferior to arthroscopic partial meniscectomy.
(more…)
Victor A. van de Graaf, MD
OLVG Ziekenhuis
Amsterdam
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Although meniscal surgeries are among the most frequently performed surgical procedures in orthopedic surgery, until just recently there were hardly any randomized trials proving its superiority over conservative treatment.
In this randomized clinical trial, including 321 patients with non-obstructive (e.g. no locking of the knee joint) meniscal tears, we found physical therapy non-inferior to arthroscopic partial meniscectomy.
(more…)