Access to capital enables practitioners to adopt innovative care delivery models such as telemedicine, remote patient monitoring, and preventive health...
Author Interviews, Mental Health Research, Pharmaceutical Companies / 14.01.2024
New study finding $14.2 million in undisclosed conflicts of interest in the “bible” of psychiatry (DSM-5-TR) published in the British Medical Journal
MedicalResearch.com Interview with:
 Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.
(more…)
Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.
(more…)
 Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.
(more…)
Lauren C. Davis, MBS
Department of Medical Education
Geisinger Commonwealth School of Medicine
Scranton, PA 19409
MedicalResearch.com: What is the background for this study?
Response: Financial conflicts of interest (COIs) resulting from ties between academia and industry have been under scrutiny for their potential to hinder the integrity of medical research. COIs can lead to implicit bias, compromise the research process, and erode public trust (1-6). The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), standardizes symptom criteria and codifies psychiatric disorders. This manual contributes to the approval of new drugs, extensions of patent exclusivity, and can influence payers and mental health professionals seeking third-party reimbursements. Given the implications of the DSM on public health, it is paramount that it is free of industry influence. Previous research has shown a high prevalence of industry ties among panel and task force members of the DSM-IV-TR and DSM-5, despite the implementation of a disclosure policy for the DSM-5 (7,8). This study (9) determined the extent and type of COIs received by panel and task-force members of the DSM-5-TR (2022) (10). As the DSM-5-TR did not disclose COI, we used the Center for Medicare and Medicaid Services Open Payments (OP) database (11) to quantify them.
(more…)
Author Interviews, Education, JAMA, Pharmaceutical Companies / 06.07.2022
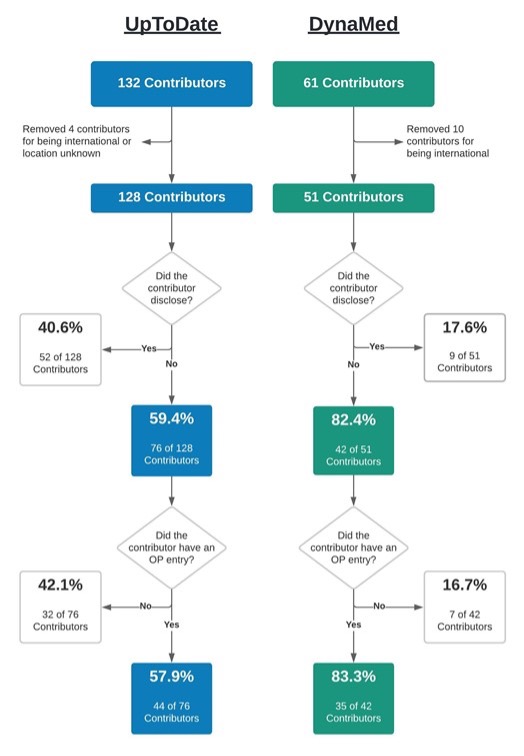
Geisinger Study Found 79 Physician Contributors to UpToDate and DynaMed with Potential Conflicts of Interest of Nearly $8 Million
MedicalResearch.com Interview with:
SooYoung VanDeMark, MBS
Geisinger Commonwealth School of Medicine
Scranton, Pennsylvania
MedicalResearch.com: What is the background for this study?
Response: Health care providers utilize subscription-based, point-of-care databases such as DynaMed and UpToDate to provide clinical care guidance and remain current on the latest evidence-based findings. Both of these websites maintain this content through a cadre of physician contributors who write and edit articles for these sites. These physician contributors are required to self-report any conflicts of interest (COI) as outlined by the respective policies on each website. However, prior COI research into similarly self-regulated areas, such as medical and pharmacology textbooks, and clinical practice guidelines, has found both appreciable potential COI and inconsistencies between self-reported and industry mandated disclosures (1-3).
This study (4) explored the accuracy of physician contributors to DynaMed and UpToDate by comparing their self-reported disclosure status with the financial remunerations they received from the healthcare industry (e.g., pharmaceutical companies) as reported to the U.S. Centers for Medicare and Medicaid Services’ Open Payments database. Physician contributors who reported “nothing to disclose” on their respective article topic but had an entry on Open Payments for having received money from industry, were classified as discordant and, thus, as having the potential for a COI. Additionally, total remuneration, gender, and payment category were investigated more in depth for each database.
(more…)
Author Interviews, Health Care Systems / 14.04.2022
High Rates of Financial Conflict-of-Interest Non-Disclosure in High-Impact US Medical Journals
MedicalResearch.com Interview with:
James H. Baraldi
University of Pittsburgh
MedicalResearch.com: What is the background for this study?
Response: Researchers investigating pharmaceuticals and medical devices in randomized controlled trials (RCTs) often receive payments from the manufacturers of these investigational products. In many cases these payments are not dedicated to the express purpose of research, but rather consist of consulting fees and compensation for travel and lodging and food and beverage. As part of the 2010 Affordable Care Act, the US government passed the Physician Payment Sunshine Act to increase transparency of this type of funding. The law required manufacturers reimbursed by Medicare, Medicaid, or the Children’s Health Insurance Program to disclose to the Centers for Medicare and Medicaid Services information regarding investigator payments. This information became freely and publicly available on the Open Payments website with the earliest data from 2013. Not only have the pharmaceutical and medical device manufacturers disclosed the investigators’ payment information, but the investigators themselves have had to do so in accordance with the requirements of the journals in which they publish their findings or in accordance with the requirements of the International Committee of Medical Journal Editors (ICMJE).
(more…)
Medicine is ever evolving, but it might surprise you to hear how far we’ve come even since the turn of the century. Advancements in technology have allowed for some amazing upgrades in medicine that could only be imagined in sci-fi movies before, and new developments in drugs have vastly increased the average life expectancy, from 77.74 in 2000 to a high of 81.3 in 2014. Read on to find out more about our top picks for the most influential advancements in medicine.
Information technology
An often overlooked but greatly impactful aspect of medicine, information technology has allowed for the smooth and faster running of hospitals. Like every other aspect of life, technology has infiltrated hospitals and GPs at a basic and far-reaching level, allowing for safer and more secure running of hospitals as well as aiding diagnosis earlier and minimally invasive procedures to create less pain and quicker healing.
Rather than sifting through filing rooms for that one patient, staff can access a patient’s file on cloud storage, where it is free from other prying eyes. Remote consultations allow for neither patient or doctor to travel to do a consultation, and an encyclopedia of symptoms and treatments are available at doctors’ fingertips.
Technology has taken the routine and tedious aspects of patient care out of the equation, or at least streamlined it, so that doctors can focus on their patients. Filing, record maintenance and other routine tasks, are all done quickly with the help of apps and cloud storage. Streamlining processes like no exam life insurance allows for doctors to focus on the care of their patients while you offer other evidence like family history and pre-existing conditions.
Doctors are working faster, patients get seen quicker, their prescriptions are issued sooner.
(more…)
Author Interviews, Education, Gender Differences, Neurology, UC Davis / 27.01.2020
Dean of UC Davis Discusses How To Encourage More Women To Become Neurologists
MedicalResearch.com Interview with:
Allison Brashear, M.D., M.B.A.
Dean, UC Davis School of Medicine
MedicalResearch.com: What is the background for this study? Why is the demand for neurology services and neurologists increasing?
Response: The American Academy of Neurology estimates that by 2025 the number of neurologists in practice will increase to 18,060 but some 3,400 more will be needed to meet the demand for their services. The 58% increase in the number of residency positions in the National Resident Matching Program since 2008 also reflects the growing demand. The higher prevalence of neurologic conditions, aging U.S. population and more patients having access to the health care coverage are the major driving forces. (Note: source of NRMP neurology trend data comes from a physician/resident forum posted May 2019 https://forums.studentdoctor.net/threads/growth-trends-in-neurology-residency-positions.1375918/)
MedicalResearch.com: Why is neurology included among the less desirable fields of medicine (similar to nephrology, infectious disease, endocrinology etc.) for medical students and residents to pursue? Why is burnout and dissatisfaction so high?
Response: According to the American Academy of Neurology, a minority of medical students choose to train in neurology each year, with approximately 3.1% matching into a neurology residency in 2018. The newer generations of neurologists value lifestyle and time off work more than their predecessors.
According to a recent American Medical Association survey, neurology tied with critical care as the medical specialty with the highest stress levels and burnout. Too many administrative tasks, too many hours at work, increased computerization of practice and insufficient compensation were among the top causes of burnout.
(more…)
Author Interviews, Dermatology, Education, Gender Differences, JAMA, Race/Ethnic Diversity / 08.01.2020
Minorities Still Underrepresented in Dermatology Faculty
MedicalResearch.com Interview with:
Imam Xierali, PhD
Associate Professor / UT Southwestern Medical Center
Dallas, Texas
MedicalResearch.com: What is the background for this study?
Response: Despite the continued efforts in academic medicine to increase the representation of women and minorities underrepresented in medicine (URM), there is a lack of information on trends in dermatology department faculty diversity and how they compare with those in other clinical departments.
(more…)
Author Interviews, Infections / 20.12.2019
Domesticated Animals Facilitate Spread of Viruses from Wildlife to Humans
MedicalResearch.com Interview with:
Konstans Wells, PhD
Lecturer in Biosciences
Swansea University
MedicalResearch.com: What is the background for this study?
Response: Cross‐species transmission of harmful viruses between animals and humans is a major source of infectious diseases and a considerable global public health burden. We assessed patterns of virus sharing among a large diversity of mammals, including humans and domestic species.
(more…)
Author Interviews, C. difficile, Gastrointestinal Disease / 20.12.2019
Asymptomatic Patients Carry C. difficile Bacteria for Deadly Diarrhea Into Hospital
MedicalResearch.com Interview with:
Sarah W. Baron, M.D
Assistant Professor
Division of Hospital Medicine
Department of Medicine, Montefiore Medical Center
Bronx, New York
MedicalResearch.com: What is the background for this study?
Response: We know that C. difficile can be a deadly and highly infectious disease but that it has been difficult to control. We also know that some people carry C. difficile in their body without symptoms but can still spread the organism or become sick with it themselves at some point in the future.
This study attempted to answer two main questions:
1. First, how many patients coming into a large, urban academic medical center carried the organism C. difficile without any symptoms and
2. How many of those carriers without symptoms then went on to have the symptoms of C. difficile within 6 months? (more…)
Author Interviews, Cost of Health Care, JAMA, Primary Care / 11.12.2019
Health Care Spending Increasing But Not On Primary Care
MedicalResearch.com Interview with:
Julie Reiff BA
Researcher
Health Care Cost Institute
MedicalResearch.com: What is the background for this study?
Response: Prior studies have attempted to define primary care spending and quantify such spending. Using definitions from the Milbank Memorial Fund, we used Health Care Cost Institute data to calculate primary care utilization and spending among those age 0-64 with employer-sponsored insurance.
(more…)
Author Interviews, Education, Neurology, NYU / 17.05.2019
Neurology Residents Learn to Identify Physician Burnout Through Simulation
MedicalResearch.com Interview with:
Dr. Rebecca Stainman
Dr. Arielle Kurzweil MD
Adult Neurology Program Director
New York University School of Medicine
NYU Langone Health
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Physician burnout is prevalent. Neurologists have among the highest burnout rates, ranked third among specialties in a 2011 study, and over half of US Neurologists report at least 1 symptom of burnout in a 2016 survey. Efforts to address burnout in training programs have mostly been aimed at implementing wellness curricula and offering mental health resources.
Training neurology residents to effectively identify, address, and help impaired colleagues is equally crucial in these efforts, yet there is a paucity of literature on this topic. We used simulation as a means of addressing this topic, via identifying and addressing an impaired colleague through an objective structured clinical examination (OSCE). (more…)
Author Interviews, Diabetes, JAMA, Technology / 18.04.2019
Most Diabetes Apps Do Not Provide Real Time Decision Support (yet)
MedicalResearch.com Interview with:
Associate Professor Josip Car
MD, PhD, DIC, MSc, FFPH, FRCP (Edin)
Associate Professor of Health Services Outcomes Research,
Director, Health Services Outcomes Research Programme and Director
Centre for Population Health Sciences
Principal Investigator, Population Health & Living Laboratory
MedicalResearch.com: What is the background for this study?
Response: In 2018, almost 8% of people with diabetes who owned a smartphone used a diabetes app to support self-management. Currently, most apps are not regulated by the US Food and Drug Administration (FDA). We downloaded and assessed 371 diabetes self-management apps, to see if they provided evidence-based decision support and patient education. (more…)
Author Interviews, Cognitive Issues, Memory, University Texas / 16.04.2019
Brain Training Can Strengthen Cognitive Function in Patients With Mild Impairment
MedicalResearch.com Interview with:
Dr. Sandra Bond Chapman PhD
Founder and Chief Director, Center for BrainHealth,
Co-Leader, The BrainHealth Project
University of Texas, Dallas
MedicalResearch.com: What is the background for this study?
Response: Finding effective treatments to reverse or slow rates of cognitive decline for those at risk for developing dementia is one of the most important and urgent challenges of the 21st century.
Brain stimulation is gaining attention as a viable intervention to increase neuroplasticity when used in isolation or when combined with cognitive training regimens. Given the growing evidence that certain cognitive training protocols, such as SMART, benefit people with Mild Cognitive Impairment (MCI), a population that is vulnerable to Alzheimer’s disease, we were interested in exploring whether we could further increase the gains from cognitive training (i.e., SMART) when the training was preceded by brain stimulation using tDCS. (more…)
Author Interviews, Cost of Health Care, Hospital Readmissions, JAMA, Outcomes & Safety / 16.04.2019
Changes in Medicare’s Hospital Readmissions Reduction Program Affect Poor and Low Poverty Hospitals Differently
MedicalResearch.com Interview with:
Karen Joynt Maddox, MD, MPH
Assistant Professor of Medicine
Washington University Brown School of Social Work
MedicalResearch.com: What is the background for this study?
Response: Medicare’s Hospital Readmissions Reduction Program has been controversial, in part because until 2019 it did not take social risk into account when judging hospitals’ performance. In the 21st Century Cures Act, Congress required that CMS change the program to judge hospitals only against other hospitals in their “peer group” based on the proportion of their patients who are poor. As a result, starting with fiscal year 2019, the HRRP divides hospitals into five peer groups and then assesses performance and assigns penalties. (more…)
Author Interviews, Brigham & Women's - Harvard, Gender Differences, JAMA, Surgical Research / 16.04.2019
Home Responsibilities Encourage Physician Mothers in Procedural Specialties To Consider Career Change
MedicalResearch.com Interview with:
Nelya Melnitchouk, MD,MSc
Director, Program in Peritoneal Surface Malignancy, HIPEC
Dr. Melnitchouk is an associate surgeon at Brigham and Women’s Hospital (BWH) and Brigham and Women’s Faulkner Hospital (BWFH) and
instructor of surgery at Harvard Medical School.
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Current literature on women in surgery show that female physicians, particularly those in procedural specialties, face many challenges in balancing responsibilities between work and home. We hypothesized that these challenges may affect career satisfaction more negatively for physician mothers in procedural specialties than those in nonprocedural specialties.
In our study, we found that physician mothers in procedural specialties who had more domestic responsibilities were more likely to report a desire to change careers than those in nonprocedural specialties. (more…)
Author Interviews, BMJ, Heart Disease, Karolinski Institute / 11.04.2019
Stress from Traumatic Events Linked to Increased Risk of Heart Disease
MedicalResearch.com Interview with:
Huan Song, PhD
Center of Public Health Sciences, Faculty of Medicine,
University of Iceland, Reykjavík, Iceland
Department of Medical Epidemiology and Biostatistics
Karolinska Institutet, Stockholm, Sweden
MedicalResearch.com: What is the background for this study?
Response: Cardiovascular disease (CVD) presents a group of diseases that are common and sometimes fatal in general population. The possible role of stress-related disorders in the development of CVD has been reported. However, the main body of the preceding evidence was derived from male samples (veterans or active-duty military personnel) focusing mainly on posttraumatic stress disorder (PTSD) or self-reported PTSD symptoms. Data on the role of stress-related disorders in CVD in women were, until now, limited. Although incomplete control for familial factors and co-occurring psychiatric disorder, as well as the sample size restriction, limit the solid inference on this association, especially for subtypes of CVD.
(more…)
Author Interviews, Opiods / 09.04.2019
Waivers to Allow PAs and NPs to Prescribe Buprenorphine Vary by State
MedicalResearch.com Interview with:
Joanne Spetz, PhD
Professor
Philip R. Lee Institute for Health Policy Studies
San Francisco, CA 94143-0936
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Medication treatment is an important component of treatment for opioid use disorder. Buprenorphine has been the focus of policies designed to increase access to treatment and is the most widely-used medication due to well-established evidence of its efficacy and its accessibility outside licensed narcotics treatment programs. The most common brand name for this medication is Suboxone.
There is a shortage of providers authorized to prescribe it, in part because only physicians were permitted to obtain waivers from the Drug Enforcement Agency to prescribe it outside of licensed narcotics treatment programs until the opioid bill of 2016. That bill granted nurse practitioners (NPs) and physician assistants (PAs) the ability to apply for waivers. However, in states that require NPs and/or PAs to be supervised by or collaborate with a physician, there are additional requirements regarding the training of the physician before the NP or PA can apply for a waiver. This affects nearly half of states for NPs, and all states for PAs.
We found that the average percentage of NPs with waivers was 5.6% in states that do not require physician supervision, but only 2.4% in more restrictive states. Even after adjusting for other factors, we found that the percentage of NPs with waivers was 75% higher when physician oversight is not required. We didn’t find a similar result for PAs, probably because they must have physician oversight in all states. (more…)
Author Interviews, Diabetes, Genetic Research, Heart Disease, Nature / 02.04.2019
Shorter Individuals at Greater Risk of Heart Disease
MedicalResearch.com Interview with:
Eirini Marouli
William Harvey Research Institute
Barts and The London School of Medicine and Dentistry, Queen Mary University of London, London
MedicalResearch.com: What is the background for this study?
Response: Epidemiological studies suggest that shorter stature is associated with increased risk of coronary artery disease (CAD) or type 2 diabetes (T2D). It is not clear though whether these associations are causal or there are other factors mediating these effects. When randomized trials are inappropriate or impossible, we can use Mendelian Randomisation as a good alternative to study the causal relationship between a trait and a disease. Here, we examined over 800 places in the human genome known to be associated with adult height and evaluated how genetically predicted height can affect the risk of CAD or T2D. Furthermore, we evaluated the role of several risk factors including, cholesterol, triglycerides, blood pressure, body mass index, fat percentage, socio-economic parameters including education and income as well as lung function. Lung function was assessed by spirometry measures including FEV1: forced expiratory volume in 1 second, FVC: forced vital capacity.
(more…)
Author Interviews, Cancer Research, FDA, JAMA / 01.04.2019
Cancer Drug Trials: Does Changing the Endpoint from Overall Survival Hasten the Approval Process?
MedicalResearch.com Interview with:
Emerson Chen, MD
Chief Fellow, Hematology-Oncology, PGY-6
Oregon Health & Science University
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Many cancer drugs are approved annually giving the appearance of innovation; however, some drugs may have been approved because of a lower bar. Use of lesser endpoints like response rate (how tumor shrinks) and progression-free survival (how tumor has delayed growth) have been proposed to speed trials when compared against traditional endpoints like overall survival (how long patients might live).
Using published trials that led to cancer drug approval from 2006 to 2017, we estimated how long it would take to get each of these three endpoints across all cancer drugs and indications to see how much time we could save by using these weaker but faster endpoints.
We see that many trials using overall survival used less time than anticipated, and many trials using response rate or progression-free survival actually took quite a bit of time. In part that is due to researchers needing to document the duration of the response. But, whatever the reason, the time to get each of the three endpoints is actually more similar than different, and we estimate that our current use of these faster endpoints are saving us only 11 months compared to using only overall survival.
(more…)
Author Interviews, Cancer Research, Cannabis, End of Life Care, NYU / 28.03.2019
Cancer Patients Use THC and CBD Differently Than Other Medical Marijuana Patients
MedicalResearch.com Interview with:
Arum Kim, MD
Assistant Professor
Medicine and Rehabilitation Medicine
NYU School of Medicine
Director of the Supportive Oncology Program
Perlmutter Cancer Center
MedicalResearch.com: What is the background for this study?
Response: There is increasing interest in medical marijuana and its applications for patients with cancers. Despite increasing access, little is known regarding doses of cannabinoids - specifically delta-8-tetrahydrocannabinol (delta-8-THC) and cannabidiol (CBD), methods of drug delivery, and differences in patterns of use between cancer and non-cancer patients.
(more…)
AACR, Author Interviews, Cancer Research, Dental Research, Pancreatic, Race/Ethnic Diversity / 28.03.2019
Tooth Loss Linked To Greater Risk of Pancreatic Cancer Among African American Women
MedicalResearch.com Interview with:
Julie R. Palmer, ScD
Professor, Boston University School of Medicine
Associate Director, Slone Epidemiology Center at Boston University
Boston, MA 02118
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Since 1995, 59,000 African American women from all regions of the U.S. have participated in a Boston University research study of the health of Black women. Study participants complete mailed or online questionnaires every two years.
Our major goal is to identify modifiable risk factors for cancers and nonmalignant conditions that disproportionately affect African Americans (e.g., pancreatic cancer, early-onset breast cancer, type 2 diabetes, uterine fibroids). The reasons for the higher incidence of pancreatic cancer in African Americans relative to non-Hispanic White women in the U.S. are unknown.
I was aware that several recent studies in predominantly White populations had observed a higher incidence of pancreatic cancer in those who had reported poor oral health and wondered whether the higher prevalence of poor oral health among African Americans could play a role in their higher incidence of pancreatic cancer. We had already asked about gum disease, periodontal disease, and adult tooth loss in several rounds of data collection.
After rigorous analysis, we found that women who reported any adult tooth loss had about two times the risk of future development of pancreatic cancer compared with those who had no tooth loss and had never reported periodontal disease.
The estimated risk was even greater for those who had lost five or more teeth. A similar association was observed for reports of periodontal disease, but the association was not statistically significant.
(more…)
Accidents & Violence, Alzheimer's - Dementia, Author Interviews, JAMA, Mental Health Research / 28.03.2019
Criminal and Socially Inappropriate Behaviors Could Be Signs of Dementia
MedicalResearch.com Interview with:
Madeleine Liljegren, MD
Division of Oncology and Pathology
Department of Clinical Sciences
Lund University Lund, Sweden
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: We know from former studies including patients with a clinical diagnosis of dementia, that criminal and socially inappropriate behaviors can be signs of dementia, sometimes even the first signs of a neurodegenerative disorder.
We wanted to study this relatively large (n=220) cohort of neuropathologically verified Alzheimer disease (AD) and frontotemporal dementia (FTD) patients, who had been followed clinically by specialists in cognitive medicine or geriatric psychiatry during their disease period, to see if we could confirm results from previous studies.
In this paper, we further wanted to study potential differences regarding protein pathology and criminal behavior in frontotemporal dementia patients. This has, to our knowledge, never been done before.
(more…)
Author Interviews, Diabetes, Heart Disease, UCSD / 28.03.2019
Gene Transfer Improved Cardiac Function in Diabetic Mouse Model
MedicalResearch.com Interview with:
H. Kirk Hammond, MD
Professor of Medicine at University of California
San Diego
Basic research scientist and cardiologist
San Diego Veterans' Affairs Healthcare System
Dr. Hammond is winner of the 2017 William S. Middleton Award – the highest research honor in the U.S. Department of Veterans Affairs
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Worldwide, 9% of adults have diabetes, predominantly due to insulin resistance, known as Type 2 diabetes. It is associated with obesity and diets high in fat and carbohydrates. In this gene transfer study we showed that a single injection of a vector encoding a natural hormone (urocortin 2, Ucn2) increased glucose disposal and improved heart function in a model of diet-induced Type 2 diabetes in mice.
(more…)
Author Interviews, Cost of Health Care, End of Life Care, Medicare, Science / 06.07.2018
Predicting Death is Difficult, Making it Difficult To Save Money on End of Life Care
MedicalResearch.com Interview with:
Amy Finkelstein PhD
John & Jennie S. MacDonald Professor of Economics
MIT Department of Economics
National Bureau of Economic Research
Cambridge MA 02139
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Although only 5% of Medicare beneficiaries die in a given year, they account for almost 25% of Medciare spending.
This fact about high end of life spending has been constantly used to refer to inefficiency of the US healthcare system. A natural observation is that the fact is retrospective, and it motivated us to explore a prospective analog, which would take as an input the probability of someone dying in a given year rather than her realized outcome. We therefore used machine learning techniques to predict death, and somewhat to our surprise we found that at least using standardized and detailed claims-level data, predicting death is difficult, and there are only a tiny fraction of Medicare beneficiaries for whom we can predict death (within a year) with near certainty.
Those who end up dying are obviously sicker, and our study finds that up to half of the higher spending on those who die could be attributed to the fact that those who die are sicker and sick individuals are associated with higher spending. (more…)
Author Interviews, Education, JAMA / 04.06.2018
Is More Supervision of Medical Residents Always Better for Patient Care?
MedicalResearch.com Interview with:
Kathleen M. Finn MD, MPhil
Christiana Iyasere MD, MBA
Division of General Internal Medicine
Department of Medicine
Massachusetts General Hospital, Boston
MedicalResearch.com: What is the background for this study?
Response: While the relationship between resident work hours and patient safety has been extensively studied, little research evaluates the role of attending supervision on patient safety. Beginning with the Bell Commission there have been increased calls for enhanced resident supervision due to patient safety concerns. At the same time, with the growth of the hospitalist movement more faculty physicians join daily resident work rounds under the assumption that increased supervision is better for patient safety and resident education. However, we know that supervision is a complex balancing act, so we wanted to study whether these assumptions were true. On the one hand patient safety is important, but on the other adult learning theory argues residents need to be challenged to work beyond their comfort level. Importantly, being pushed beyond your comfort level often requires appropriate space between teacher and learner. To investigate the role of attending supervision on patient safety and resident learning we studied the impact of two levels of physician supervision on an inpatient general medical team.
Twenty-two teaching faculty were randomized to either direct supervision of resident teams for patients previously known to the team vs usual care where they did not join rounds but rather discussed the patients later with the team. Faculty participated in both arms of the study, after completing the first arm they then crossed over to the other arm; each faculty member participated in the study for a total of 4 weeks.
(more…)
Author Interviews, Duke, Education, Heart Disease, JAMA / 01.06.2018
Female Residents Do Not Perceive Cardiology As Conducive To Work-Family Balance
MedicalResearch.com Interview with:
Pamela S. Douglas, MD, MACC, FASE, FAHA
Ursula Geller Professor of Research in Cardiovascular Disease
Duke University School of Medicine
Durham, NC 27715
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: For any profession to succeed, it needs to attract top talent. We surveyed internal medicine residents to find out what they valued most in their professional development, how they perceived cardiology as field and how these two areas are associated with their choosing a career in cardiology or another specialty.
We found that trainees were seeking careers that had stable hours, were family friendly and female friendly, while they perceived cardiology to have adverse work conditions, interfere with family life and to not be diverse. We were able to predict career choice with 89-97% accuracy from these responses; the predictors are mix of things that attract to cardiology and those that are deterrents.
For men, the attractors outnumber the deterrents, for women its just the opposite.
(more…)
Author Interviews, Cost of Health Care, JAMA / 05.01.2018
Male Physicians Receive More Money From Industry Than Women Doctors
MedicalResearch.com Interview with:
 Kathryn R. Tringale, MAS
Department of Radiation Medicine and Applied Sciences
University of California San Diego, La Jolla
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Financial relationships between biomedical industry and physicians are common, and previous work has investigated the potential conflicts of interest that can arise from these interactions.
Data show that even small payments in the form of industry sponsored lunches can influence physician prescribing patterns. Given the concern for the potential influence of biomedical industry over practice patterns and potentially patient care, the Open Payments program was implemented under the Affordable Care Act to shed light on these interactions and make reports of these financial transactions publicly available. We recently published a paper in JAMA on industry payments to physicians that found that men received a higher value and greater number of payments than women physicians and were more likely to receive royalty or licensing payments when grouped by type of specialty (surgeons, primary care, specialists, interventionalists).
The purpose of the Research Letter discussed here was to further examine differences in the value of payments received by male and female physicians within each individual specialty. The main takeaway from this study is that male physicians, across almost every specialty, are receive more money from biomedical industry compared to female physicians. At first glance, this finding can be interpreted as merely another example of gender disparities in the workplace, which we have seen before with gender gaps in physician salaries and research funding. Indeed, this gender gap may be a product of industry bias leading to unequal opportunity for women to engage in these profitable relationships. Alternatively, these data may be more representative of gender differences in physician decision-making. Previous data has shown that industry engagement can lead to changes in practice patterns, so maybe female physicians acknowledge these conflicts of interest and actively choose not to engage with industry. Unfortunately, we cannot tease out these subtleties from our results, but our paper does reveal a remarkable gender difference among physician engagement with industry. With this being said, whether male or female, everyone needs a bit of help sometimes. The use of loans is a possibility for many people who need a little financial assistance. Regardless of whether men are getting paid a little more than women, they may all need help just as equally. The type of loans that would be worth looking into if this is your current situation is physician loans, which basically allows medical professionals to purchase a home with a low/little down payment while avoiding mortgage insurance. A little bit of help goes a long way, especially when it involves your future.
(more…)
Kathryn R. Tringale, MAS
Department of Radiation Medicine and Applied Sciences
University of California San Diego, La Jolla
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Financial relationships between biomedical industry and physicians are common, and previous work has investigated the potential conflicts of interest that can arise from these interactions.
Data show that even small payments in the form of industry sponsored lunches can influence physician prescribing patterns. Given the concern for the potential influence of biomedical industry over practice patterns and potentially patient care, the Open Payments program was implemented under the Affordable Care Act to shed light on these interactions and make reports of these financial transactions publicly available. We recently published a paper in JAMA on industry payments to physicians that found that men received a higher value and greater number of payments than women physicians and were more likely to receive royalty or licensing payments when grouped by type of specialty (surgeons, primary care, specialists, interventionalists).
The purpose of the Research Letter discussed here was to further examine differences in the value of payments received by male and female physicians within each individual specialty. The main takeaway from this study is that male physicians, across almost every specialty, are receive more money from biomedical industry compared to female physicians. At first glance, this finding can be interpreted as merely another example of gender disparities in the workplace, which we have seen before with gender gaps in physician salaries and research funding. Indeed, this gender gap may be a product of industry bias leading to unequal opportunity for women to engage in these profitable relationships. Alternatively, these data may be more representative of gender differences in physician decision-making. Previous data has shown that industry engagement can lead to changes in practice patterns, so maybe female physicians acknowledge these conflicts of interest and actively choose not to engage with industry. Unfortunately, we cannot tease out these subtleties from our results, but our paper does reveal a remarkable gender difference among physician engagement with industry. With this being said, whether male or female, everyone needs a bit of help sometimes. The use of loans is a possibility for many people who need a little financial assistance. Regardless of whether men are getting paid a little more than women, they may all need help just as equally. The type of loans that would be worth looking into if this is your current situation is physician loans, which basically allows medical professionals to purchase a home with a low/little down payment while avoiding mortgage insurance. A little bit of help goes a long way, especially when it involves your future.
(more…)
 Kathryn R. Tringale, MAS
Department of Radiation Medicine and Applied Sciences
University of California San Diego, La Jolla
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Financial relationships between biomedical industry and physicians are common, and previous work has investigated the potential conflicts of interest that can arise from these interactions.
Data show that even small payments in the form of industry sponsored lunches can influence physician prescribing patterns. Given the concern for the potential influence of biomedical industry over practice patterns and potentially patient care, the Open Payments program was implemented under the Affordable Care Act to shed light on these interactions and make reports of these financial transactions publicly available. We recently published a paper in JAMA on industry payments to physicians that found that men received a higher value and greater number of payments than women physicians and were more likely to receive royalty or licensing payments when grouped by type of specialty (surgeons, primary care, specialists, interventionalists).
The purpose of the Research Letter discussed here was to further examine differences in the value of payments received by male and female physicians within each individual specialty. The main takeaway from this study is that male physicians, across almost every specialty, are receive more money from biomedical industry compared to female physicians. At first glance, this finding can be interpreted as merely another example of gender disparities in the workplace, which we have seen before with gender gaps in physician salaries and research funding. Indeed, this gender gap may be a product of industry bias leading to unequal opportunity for women to engage in these profitable relationships. Alternatively, these data may be more representative of gender differences in physician decision-making. Previous data has shown that industry engagement can lead to changes in practice patterns, so maybe female physicians acknowledge these conflicts of interest and actively choose not to engage with industry. Unfortunately, we cannot tease out these subtleties from our results, but our paper does reveal a remarkable gender difference among physician engagement with industry. With this being said, whether male or female, everyone needs a bit of help sometimes. The use of loans is a possibility for many people who need a little financial assistance. Regardless of whether men are getting paid a little more than women, they may all need help just as equally. The type of loans that would be worth looking into if this is your current situation is physician loans, which basically allows medical professionals to purchase a home with a low/little down payment while avoiding mortgage insurance. A little bit of help goes a long way, especially when it involves your future.
(more…)
Kathryn R. Tringale, MAS
Department of Radiation Medicine and Applied Sciences
University of California San Diego, La Jolla
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Financial relationships between biomedical industry and physicians are common, and previous work has investigated the potential conflicts of interest that can arise from these interactions.
Data show that even small payments in the form of industry sponsored lunches can influence physician prescribing patterns. Given the concern for the potential influence of biomedical industry over practice patterns and potentially patient care, the Open Payments program was implemented under the Affordable Care Act to shed light on these interactions and make reports of these financial transactions publicly available. We recently published a paper in JAMA on industry payments to physicians that found that men received a higher value and greater number of payments than women physicians and were more likely to receive royalty or licensing payments when grouped by type of specialty (surgeons, primary care, specialists, interventionalists).
The purpose of the Research Letter discussed here was to further examine differences in the value of payments received by male and female physicians within each individual specialty. The main takeaway from this study is that male physicians, across almost every specialty, are receive more money from biomedical industry compared to female physicians. At first glance, this finding can be interpreted as merely another example of gender disparities in the workplace, which we have seen before with gender gaps in physician salaries and research funding. Indeed, this gender gap may be a product of industry bias leading to unequal opportunity for women to engage in these profitable relationships. Alternatively, these data may be more representative of gender differences in physician decision-making. Previous data has shown that industry engagement can lead to changes in practice patterns, so maybe female physicians acknowledge these conflicts of interest and actively choose not to engage with industry. Unfortunately, we cannot tease out these subtleties from our results, but our paper does reveal a remarkable gender difference among physician engagement with industry. With this being said, whether male or female, everyone needs a bit of help sometimes. The use of loans is a possibility for many people who need a little financial assistance. Regardless of whether men are getting paid a little more than women, they may all need help just as equally. The type of loans that would be worth looking into if this is your current situation is physician loans, which basically allows medical professionals to purchase a home with a low/little down payment while avoiding mortgage insurance. A little bit of help goes a long way, especially when it involves your future.
(more…)
Author Interviews, Cost of Health Care, JAMA, NIH / 17.01.2017
Conflicts of Interest In Medical Guideline Committees Underreported
MedicalResearch.com Interview with: [caption id="attachment_31328" align="alignleft" width="200"] Dr. Akilah Jefferson[/caption] Akilah Jefferson, MD, MSc Postdoctoral Fellow, Clinical Center, Department of Bioethics Clinical Fellow, Allergy...
Author Interviews, Education, JAMA / 06.12.2016
MILESTONE Ratings of Medical Residents Better Able To Distinguish Competence
MedicalResearch.com Interview with:
Karen E. Hauer, MD, PhD
Associate Dean, Competency Assessment and Professional Standards
Professor of Medicine, UCSF
San Francisco, CA 94143
MedicalResearch.com: What is the background for this study?
Response: As part of the Accreditation Council for Graduate Medical Education (ACGME)’s Next Accreditation System, residency programs are now required to rate residents using the Milestones. Evidence of validity of Milestone ratings is needed to show whether this rating system measures meaningful aspects of residents’ practice.
In the field of internal medicine, we compared ratings of residents using the old evaluation form, the pre-2015 Resident Annual Evaluation Summary (RAES), which has a non-developmental rating scale that rates residents from unsatisfactory to superior on a 9-point scale, with developmental Milestone ratings. This was a cross-sectional study of all United States internal medicine residency programs in 2013-14, including 21,284 internal medicine residents. Milestone ratings are submitted by residency program directors working with Clinical Competency Committees. We correlated RAES and Milestone ratings by training year; correlated ratings of Medical Knowledge milestones using the two systems with American Board of Internal Medicine (ABIM) certification examination scores; and examined ratings of unprofessional behavior using the two systems.
(more…)
Author Interviews, Health Care Systems, Lancet, Mayo Clinic / 03.10.2016
What Interventions Can Reduce Epidemic Physician Burnout?
MedicalResearch.com Interview with:
Colin P. West, MD, PhD, FACP
Divisions of General Internal Medicine and Biomedical Statistics and Informatics
Departments of Internal Medicine and Health Sciences Research
Mayo Clinic
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Physician burnout has reached epidemic levels, as documented in national studies of both physicians in training and practicing physicians demonstrating burnout rates in excess of 50%. Consequences include negative effects on patient care, professionalism, physicians’ own care and safety, and the viability of health-care systems. We conducted a systematic review and meta-analysis to better understand the quality and outcomes of the literature on approaches to prevent and reduce burnout.
We identified 2617 articles, of which 15 randomized trials including 716 physicians and 37 cohort studies including 2914 physicians met inclusion criteria. Across interventions, overall burnout rates decreased from 54% to 44%, emotional exhaustion score decreased from 23.82 points to 21.17 points, and depersonalization score decreased from 9.05 to 8.41. High emotional exhaustion rates decreased from 38% to 24% and high depersonalization rates decreased from 38% to 34%.
(more…)
- 1
- 2